Are you worried you’ll have a Heart Attack or Stroke?
CIMT Testing may help
I’ve said it many times, in case you didn’t already know, cardiovascular disease is the #1 killer of men and women in both the United States and the world.
I work in the Emergency Department (as well as my functional medicine clinic in Tulsa, OK) and I can’t tell you how many men and women come in to the ER having a heart attack and had no idea they had cardiovascular disease.
Undetected cardiovascular disease is the GREATEST RISK facing Americans today.
It gets worse. According to the AHA 2002 and 2009 Heart & Stroke Statistical Updates, cardiovascular disease increased 33% in 7 years. That’s scary!3
For every woman who dies of breast cancer, 8 women will die from cardiovascular disease (heart attacks). We are doing better with identifying and treating breast cancer as the number of deaths are decreasing. However, cardiovascular disease is increasing. More women than men over the age of 64 have hypertension. After the age of 45, hypertension risk is the same in women as it is in men. Women have more strokes than men (55,000 more per year to be exact).3
Testing for cardiovascular disease involves an evaluation of
- risk factors (lipids, family history, inflammation, genetics, etc)
- functional testing (endothelial function, pulse wave velocity, stress testing)
- structural testing (coronary calcium score, CT angiography, coronary catheterization)
Many tests for cardiovascular disease and disease risk involve population or statistical evaluations meaning that we compare, through statistical analysis, what we see in the population and what is the likelihood that population has a certain outcome. It is good for epidemiology and statistics but does NOT tell us about YOUR specific risk.
Who Should Get CIMT Testing?
The SHAPE Guideline recommends screening for all asymptomatic men age 45-75 and women age 55-75.9 The purpose is to identify and treat patients with sub-clinical cardiovascular disease just like the patients mentioned at the beginning of this article. SHAPE estimated that 50 million people in the United States should be getting this screening.
Patients with other risk factors such as hypertension, hyperlipidemia, obesity, diabetes, or metabolic syndrome should be screened at younger ages than listed above due to the fact that they are at higher risk of cardiovascular disease.
You need CIMT testing if you meet any of the following criteria:
- Men over 45 years of age
- Women over 55 years of age
- Hypertension
- Hyperlipidemia
- Obesity
- Diabetes
- Metabolic Syndrome
What is CIMT Testing?
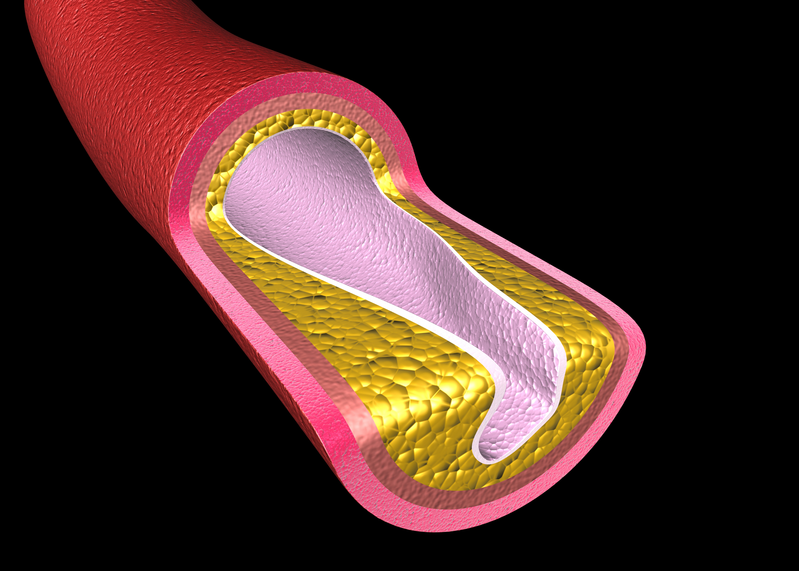
Carotid Intima Media Thickness (CIMT) Testing measures the thickness of the wall of the inner two layers of the carotid artery. It is one of the best ways to look at the structure of the carotid artery and determine future risk of Heart Attacks and Strokes.
One of the great things about carotid IMT is that it is an actual measurement of vascular disease in you. It isn’t a statistical or population based evaluation. It is actual disease. It measures the amount of plaque in the carotid artery as well as the thickness of the artery itself and it tells us about your specific risk.
CIMT testing is FDA approved and involved the use of an ultrasound to take pictures of the carotid artery in your neck. The test is painless and quick. A small amount of ultrasound gel is placed on your neck so that the ultrasound probe can accurately take the required images. The ultrasound probe is then scanned over your neck taking the images which are sent to the radiologist for analysis.
The report comes back to our office in 2-3 days and we will go over the results with you during an office visit.
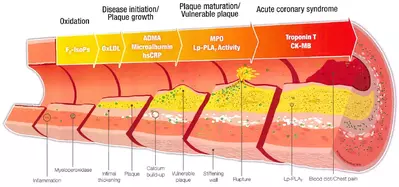
This image shows a progression of vascular disease and plaque. You’ll note that intimal thickening occurs very early in the process. That is why measuring intima media thickness in the carotid is a good idea. It allows us to qualify and quantify vascular disease specifically.
We aren’t looking at risk factors or “what is the likelihood.” We are looking at actual disease. And the thicker your CIMT the worse the disease.
Measuring CIMT allows us to detect the presence of cardiovascular disease at a very early stage in a way that most other tests do not. It allows patients to take a specific look at their cardiovascular health.
Once we identify cardiovascular disease we can begin to intervene. Once you see that you have some vascular disease you can begin to make changes.
CIMT also allows us to track our progress. We’ll put you on a plan to improve your cardiovascular health and CIMT testing will tell us if our plan is working! There aren’t many other tests that can do this. And, we can improve CIMT with proper therapy by the way.4
I don’t know if it is sad or funny but we use all kinds of screenings to identify early stage cancer in patients without any symptoms (think pap smears, colonoscopies, and mammograms to name a few) but try to get a screening test for cardiovascular disease through your regular doctor. It is very difficult because insurance doesn’t want to pay for it. Yet all forms of cancer combined account for far fewer deaths per year compared to cardiovascular disease.
What Does The Research Say?
CIMT is a well validated test. The benefits of this test are all over the medical literature. The validity of CIMT testing is well documented throughout peer reviewed medical journals.
The American Heart Association published guidelines in 2000 validating CIMT as a test for the early detection of cardiovascular disease.
CIMT Testing has been conclusively demonstrated as a surrogate endpoint for atherosclerosis, cardiovascular disease, future risk of heart attacks, future risk of stroke, future risk of TIA, and correlates well with risk factors.1
Carotid IMT is an independent predictor of vascular events in high risk patients in whom risk factors are managed clinically. One standard deviation in IMT increase was associated with increased vascular events (RR 1.57) with a high range of 2.5-6.3 from mid to high tertile.2
Carotid US is a safe and available non-invasive diagnostic tool that provides information about the carotid arteries’ characteristics and may be used for early detection of coronary artery disease as well as cardiovascular and stroke event risk stratifications.[3]
According to the Journal of the American Heart Association, CIMT is a surrogate marker of atherosclerosis.3 In other words, if your CIMT is increased then you have atherosclerosis. CIMT is a well validated predictive test for clinical coronary events. This was published in the Annals of Internal Medicine.3 Similar articles have been published in ‘Stroke’ from the Journal of the American heart Association and the Journal of the College of Cardiology.
The “2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults: A Report of t he American College of CardiologyFoundation/American Heart Association Task Force on Practice Guidelines” recommended CIMT for detection of atherosclerosis in asymptomatic patients.”7
The Mayo Clinic summarized the value of carotid IMT in its March, 2009 edition of the Mayo Clinic “Proceedings” magazine in which it stated the following: “Conclusion – A CIMT evaluation can detect subclinical vascular disease in young to middle-aged patients with low FRS and CACS of zero. These findings have important implications for vascular disease screening and the implementation of primary–prevention strategies.”8
The Screening for Heart Attack Prevention and Education (SHAPE) Task Force has recommended a new practice guideline for cardiovascular screening in the asymptomatic at-risk population. This group was comprised of leading cardiologists throughout the country. In summary, the SHAPE Guide line calls for noninvasive screening of all asymptomatic men 45-75 years of age and asymptomatic women 55–75 years of age (except those defined as very-low-risk) to detect and treat those with sub-clinical atherosclerosis. The SHAPE Report points out that “In the existing guidelines the low–risk and intermediate-risk population account for the majority of heart attacks, and only less than 20% of the total number of the events results from the high-risk population.”9
CIMT and Coronary Artery Calcium Score
The Coronary Artery Calcium Score (CACS) is a CT scan of the heart that allows quantification of calcium in the coronary arteries. The Calcium Score is a very useful test and if you have an elevated score then you can bet that you have cardiovascular disease. The CACS is a proven test useful for predicting risk of future heart attacks.
However, I have seen patients with a coronary calcium score of 0 (zero) have a heart attack a year later. It is a good test but not perfect. This test is a part of our comprehensive cardiovascular screening exam.
Coronary Artery Calcium Scoring has been available longer than CIMT testing. Therefore, it is more widely available. However, these 2 tests provide very different information.
First, the Coronary Artery Calcium Score is looking at the arteries around your heart and the CIMT is looking at the carotid arteries.
CIMT is measuring the atherosclerotic plaque in the wall of the carotid artery. The coronary artery calcium score does not look at this. It cannot detect vascular disease this early.
Coronary artery calcium scoring cannot determine plaques that are soft or mixed. CIMT does pick these up. This issue explains why I’ve seen patients have heart attacks with a normal coronary artery calcium score.
CIMT also appears to detect subclinical atherosclerosis in low-risk patients. The Journal of the American Society of Echocardiography stated “In asymptomatic patients without cardiovascular disease, CIMT and plaque assessment are more likely to revise FRS than CACS. Body mass index predicts increased CIMT in low-FRS subjects. These findings may have broad implications for screening in low–FRS subjects.”10 In other words, the CIMT may help determine risk of cardiovascular disease better than coronary artery calcium score in patients with low Framhingham Risk Scores (FRS).
Here are some additional posts on CIMT Testing:
- CIMT Testing Vs Carotid Duplex Doppler Ultrasound
- How To Improve Your CIMT Score
- How To Read Your CIMT Report
References
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, Csiba L, Desvarieux M, Ebrahim S, Fatar M, Hernandez Hernandez R, Jaff M, Kownator S, Prati P, Rundek T, Sitzer M, Schminke U, Tardif JC, Taylor A, Vicaut E, Woo KS, Zannad F, Zureik M. Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis. 2007;23(1):75-80. Epub 2006 Nov 14
Results of the Osaka Follow-Up Study for Carotid Atherosclerosis 2 (OSACA2 Study) Kitagawa K. Hougaku H. Yamagami H. Hashimoto H. Itoh T. Shimizu Y. Takahashi D. Murata S. Seike Y. Kondo K. Hoshi T. Furukado S. Abe Y. Yagita Y. Sakaguchi M. Tagaya M. Etani H. Fukunaga R. Nagai Y. Matsumoto M. Hori M. Carotid Intima-Media Thickness and Risk of Cardiovascular Events in High-Risk Patients. Cerebrovasc Dis 2007;24:35–42 (DOI:10.1159/000103114)
Lloyd-Jones D, et al. Heart Disease and Stroke Statistics—2009 Update. A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;119:e21–e181.
Wendy J. Mack, PhD; Robert H. Selzer, MS; Howard N. Hodis, MD; Joel K. Erickson, BS; Chao-ran Liu, MD; Ci-hua Liu, MD; Donald W. Crawford, MDt; David H. Blanken horn, MD, “One–Year Reduction and Longitudinal Analysis of Carotid Intima-Media Thickness Associated With Colestipol/Niacin Therapy,” Stroke, Journal of the American Heart Association, 1993;24;1779-1783.
Eric de Groot, MD, PhD; G. Kees Hovingh, MD; Albert Wiegman, MD; Pat rick Duriez, PhD; Andries J. Smit, MD, PhD; Jean-Charles Fruchart, PhD; John J.P. Kastelein, MD, PhD; “Measurement of Arterial Wall Thickness as a Surrogate Marker for Atherosclerosis.”Circulation, Journal of the American Heart Association;2004;109;33-38.
Howard N. Hodis, MD; Wendy J. Mack, PhD; Laurie La Bree, MS; Robert H. Selzer, MS; Chao-ran Liu, MD; Ci-hua Liu, MD; and Stanley P. Azen, PhD: “The Role of Carotid Arterial lntima-Media Thickness in Predicting Clinical Coronary Events” Annals of Internal Medicine, 15 February, 1998: 262-269.
STEVEN J. LESTER MD, FRCPC, MACKRAM F. ELEID, MD; BIJOYK K. HANDHERIA, MD; AND R. TODD HURST, MD, “Carotid lntima-Media Thickness and Coronary Artery Calcium Score as Indications of Subclinical Atherosclerosis,” Mayo Clinic Proceedings, March 2009;84(3):2 29-233
Philip Greenland, Joseph S. Alpert, George A. Beller, Emelia J. Benjamin, Matthew J. Budoff, Zahi A. Fayad, Elyse Foster, Mark A. Hlatky, John McB. Hodgson, Frederick G. Kushner, Michael S. Lauer, Leslee J. Shaw, Sidney C. Smith, Jr, Allen J. Taylor, William S. Weintraub, and Nanette K. Wenger, “2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines” Developed in Collaboration With the AmericanSociety of Echocardiography American Society of Nuclear Cardiology, Society of AtherosclerosisIm aging and Prevention, Society for CardiovascularAngiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance J. Am. Coll. Cardiol. 2010;56;e50-el03 originally published on line Nov 15, 2010
Morteza Naghavi, MD, Erling Falk, MD, PhD, Harvey S. Hecht, MD, Michael J Jamieson, MD, Sanjay Kaul, MD, MPH, Daniel Berman, MD, Zahi Fayad, PhD, Matthew J. Budoff, MD, John Ru mberger,MD, PhD, Tasneem Z. Naqvi, MD, Leslee J. Shaw, PhD, Ole Faergeman, MD, Jay Cohn, MD, Raymond Bahr, MD, Wolfgang Koenig, MD, PhD, Jasenka Demirovic, MD, PhD, Dan Arking, PhD, Victoria L.M.Herrera, MD, Juan Badimon, PhD, James A. Goldstein, MD, Yoram Rudy, PhD, Juhani Airaksinen, MO, Robert S. Schwartz, MD, Ward A. Riley, PhD, Robert. A. Mendes, MD, Pamela Douglas, MD, Prediman K. Shah, MD; “From Vulnerable Plaque to Vulnerable Patient – Part 111: Executive Summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force Report, 8 June 2006; The American Journal of Cardiology, 17 July 2006 (Vol. 98, Issue2 (Supplement 1), Pages 2-15).
Tasasneem Z. Naqvi, MD, FRCP, FACC, Fernando Mendoza, MD, Farhad Rafii, MD, Heidi Gransar, Maria Guerra, Norman Lepor, MD, FACC, FAHA, Daniel S. Berman, MD, FACC, FAHA, and Prediman K. Shah, MD, FACC, FAHA, Los Angeles, California, “High Prevalence of Ultrasound Detected Carotid Atherosclerosis in Subjects with Low Framingham Risk Score: Potential Implications for Screening for Subclinical Atherosclerosis.”Journal of the American Society of Echocardiography, 2010;23:809–15.
Kupetsky-Rincon EA, Uitto J. Magnesium: novel applications in cardiovascular disease–a review of the literature. Ann Nutr Metab. 2012;61(2):102-10.