We are a Functional Medicine clinic and we are constantly seeking to identify and treat the underlying cause for disease. Cardiovascular disease is the #1 killer in the world so it is a major consideration in our Tulsa, Oklahoma Functional Medicine clinic.
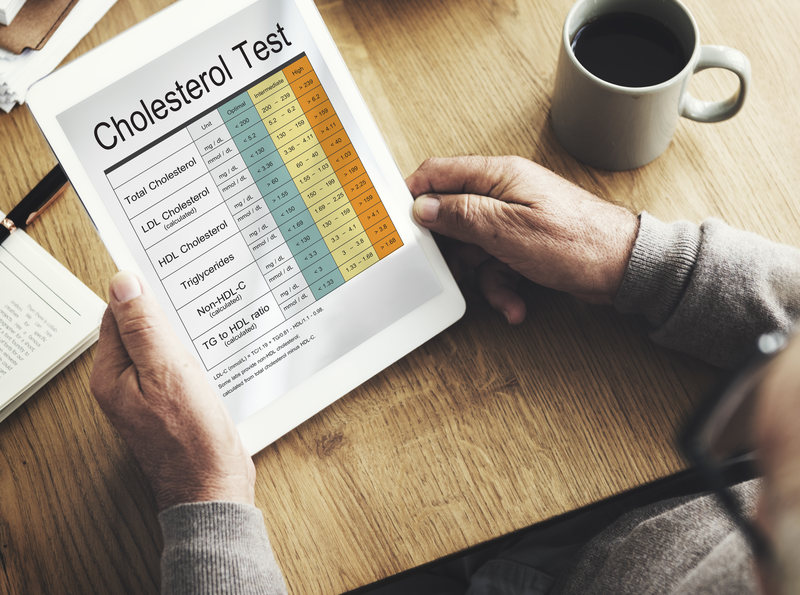
This post focuses on at what we are looking in regards to cholesterol and lipid labs as well as what to do about them. Hopefully, this will help you understand why we care about each of these topics and why we are recommending what we recommend.
The recommendations for treatment are only suggestions and it isn’t necessary to take every one of them. Patients in our Functional Medicine Tulsa clinic will get specific, directed recommendations based on the entirety of their labs and evaluation.
I often hear people talk about their cholesterol and even use it as a metric for whether or not they are healthy. However, “cholesterol” doesn’t cause cardiovascular disease.
Cholesterol is simply an essential substance for your health. It is the backbone of Vitamin D, sex hormones (testosterone, estrogen, progesterone, aldosterone, cortisol, etc), bile, myelinated structures of the brain and central nervous system, and cell membrane fluidity. You MUST have cholesterol.
 But… cholesterol is a fatty type substance and doesn’t dissolve it water (blood) so it has to have a carrier. Enter LDL.
But… cholesterol is a fatty type substance and doesn’t dissolve it water (blood) so it has to have a carrier. Enter LDL.
LDL
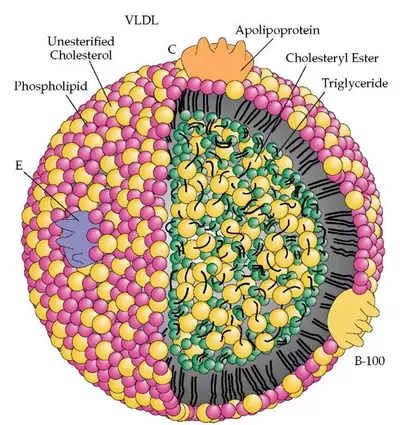
Low-Density Lipoprotein (LDL) is a molecule consisting of triglycerides, proteins, cholesterol, and phospholipids. Notice that this molecule is NOT just cholesterol. When your doctor checks your cholesterol, they are actually checking your lipoproteins.
Most people refer to this particle as the “bad” cholesterol. It isn’t bad. It is essential to life and it DOESN’T cause cardiovascular disease, heart attacks, or plaques in your arteries.
LDL is a normal, natural molecule manufactured by your body and is not harmful or detrimental (with some exceptions in extreme situations) in its native form. However, it can be altered by a number of different mechanisms. The altered LDL IS atherogenic and DOES cause cardiovascular disease.
So then, why do many doctors tell you that you have to get your LDL down? And why does the medical literature show some benefit with decreasing LDL?
It isn’t because LDL CAUSES cardiovascular disease. The traditional medical approach would make you think that but a Functional Medicine approach seeks to understand the root causes and LDL is not the root cause. But… you do have to have LDL in order to make plaque in your arteries.
Think of LDL as the building block for plaque. If you want to build a wall, you have to have bricks. No bricks, no wall. But, a pile of bricks doesn’t make a wall. Something has to put it together. The combination of inflammation, oxidative stress, and vascular immune dysfunction are the mechanisms that put the altered LDL molecules (the bricks) together to form plaque.
Another analogy I use is to think of a bon fire. In order to have a bon fire, you have to have sticks and logs arranged into a bon fire structure. You can put all the sticks and logs you want on the pile but without a spark or a flame you’ll never actually have a bon fire.
The target level for LDL is 70 mg/dL
How to decrease your LDL:
- Niacin
- Red Yeast Rice –
- Plant Sterols
- Sesame
- Tocotrienols (gamma/delta)
- Pantethine
- Citrus Bergamot
- EGCG
- Omega-3s
- Flax Seed
- Mono-Unsaturated Fatty Acids (Olive Oil)
- Garlic
- Resveratrol
- Soy
- Lycopene
- Berberine – 500mg 2-3 times daily. This is a natural PCSK9 inhibitor.
LDL-P
When you have your LDL measured they are measuring the weight of LDL in a given volume of blood. It is like saying “you have a ton of bricks” in a truck. It is measured in milligrams per deciliter (mg/dL). LDL-P is the measurement of LDL particle number. It tells you how many bricks are in the truck.
When you understand the process of atherogenesis (the formation of plaques in the arteries) then it makes absolute sense WHY the number of these particles matter. LDL particle number is what drives the risk of CVD. Also, when your LDL-P numbers are low, sdLDL (see below) becomes less of an issue. Again, it makes sense when you understand how the blood vessels create plaques. The video below should give you an idea of how the process works.
The target for LDL-P is <700 nmol/L
How to decrease your LDL-P:
- Niacin
- Omega-3s
- Berberine
- Red Yeast Rice
- Statins are only 30-50% effective for LDL-P
sdLDL (Small Dense LDL)
As mentioned in the video above, sdLDL gets through the cracks in the endothelial wall easier as it is a smaller LDL particle. Part of the problem is that this sdLDL doesn’t attach to its receptor very well so it doesn’t get taken out of circulation as it should. Thus, it floats around longer.
The smaller, denser particles get through the cracks in the endothelium and get stuck in the sub-endothelial layer. These particles are highly susceptible to oxidation. There is more information on the alteration of LDL below but the oxidation of LDL is extremely bad. Since these particles are more susceptible to oxidation, sdLDL increases the inflammatory process and predisposes to higher risk of cardiovascular disease.
If LDL-P is elevated then sdLDL is the primary driving factor for cardiovascular disease. However, once the LDL-P is optimal (<700) then sdLDL is no longer a factor.
How to increase the size of your LDL and reduce sdLDL:
- Niacin
- Omega-3s
- Plant sterols
- Water soluble fiber: psyllium
- Reduce Triglycerides to below 75 mg/dL
- Reduce refined carbohydrates
oxLDL
LDL can be altered in a number of ways such as glycation (as is the case with diabetes and elevated blood sugar), inflammation, and oxidation. Through oxidative processes (which are bad by the way) your LDL molecules become altered and creates an oxidized LDL (oxLDL).
This altered LDL particle is recognized by the immune system as abnormal or foreign. In fact, the pattern recognition receptors in your immune system identify the oxLDL as a threat in the exact same way that it identifies E. coli as a threat. That means that your body can’t differentiate between oxLDL and E. coli, an infection.
The difference between your body fighting oxLDL and E. coli is that when your body fights an infection, like E. coli, there is a finite number of the bacteria and it will usually get control of it and begin to eliminate it. The problem is that your body continues to produced oxidized LDL and continually stimulates the inflammatory process. Your body can’t ever get ahead.
Your immune system is doing what it is supposed to do. It is responding appropriately to a specific threat. However, the responses get exaggerated and out of control resulting in damage.
oxLDL is BAD stuff and tells us that there is a major problem. We want the oxLDL levels as low as we can get them. The more oxLDL you have the more inflammation it causes. That is a BAD thing!!
How to fix your oxLDL:
- Green Tea – Green Tea Extract 1 capsule twice daily. Some people will need 2 capsules twice daily. Of course, you can simply drink green tea but it will take 2-3 quarts per day in order to get enough of the EGCG.
- Olive Oil –
- CoQ10 –
- Niacin
- EGCG and other actechins
- Pantethine
- Resveratrol
- Garlic
- Tocophorols
- Oleic Acid (MUFA)
- Curcumin
- Pomegranate
- Gluathione
- Sesame
- Gamma/Delta tocotrienols
- Lycopene
- Quercetin
- Polyphenols & Flavonoids
- Citrus Bergamot
- Tangerine Extract
- Pycnogenol
As mentioned above, LDL can be altered in other ways as well. Glycation is probably the greatest threat and you can inhibit this process by supplementing with:
- Carnosine
- Pomegranate
- Histadine
- Rutin
- Organosulfur Compounds
- Morin
- Myricetin
- Kaempferol
Lp(a)
We usually refer to this one as “Lp little a.” Lp(a) is a special type of LDL particle that has a highly glycated apolipoprotein(a) (aka Apo(a)) that is bonded to ApoB100 of the LDL particle. The apolipoprotein(a) is attached to ApoB100 by a single disulfide bond. The Apo(a) is comprised of a protease domain and a series of peptide kringles (kringle repeats).
Lp(a) does not bind to the LDL receptor and it is cleared by the kidney and the liver. Some labs measure Lp(a) mass but the Lp(a)-P (particle number) correlates better with the risk of cardiovascular disease. Cardiovascular disease risk is increase 1.5-3 times if there is elevated Lp(a). Lp(a) is the “Hidden Risk” in relation to lipids for cardiovascular disease.
Basically, Lp(a) interferes with tPa (tissue plasminogen activator) which breaks down clots. Since Lp(a) interferes with it, it doesn’t break down the clots and you end up having worsening clots. That is a bad thing, especially in the artery and especially in the presence of unstable plaques in the arteries.
Elevated Lp(a) is an independent risk factor for cardiovascular disease, heart attacks, strokes, peripheral vascular disease, and blood clots (DVT). There is a linear, increased risk of these things. The higher the Lp(a) (starting at a level of 25 mg/dL) the higher the risk. Lp(a) is probably the biggest contributor to the Coronary Heart Disease Gap.
I’ve mentioned oxidized LDL and discussed its problems above. Another oxidized particle that causes a problem is oxidized phospholipid (oxPL). Lp(a) is a major carrier of these pro-inflammatory oxidized phospholipids.
Also, if you’ve had a stent in one of your coronary arteries you increase re-stenosis (your stent closing back up) 2% for every mg/dL of Lp(a). This is the case even if your other lipid levels (cholesterol levels) reach target levels.[1]
Statins actually increase Lp(a) so you want to avoid them if your Lp(a) is a problem. Trans fats increase Lp(a) as well.
The target for Lp(a) is <30 mg/dL
How to decrease your Lp(a)
- Niacin – the response is dose related. 2 grams per day decreases Lp(a) 21-40%. Start with 500mg once daily. After 2-4 weeks add a 2nd tablet each day. You can try taking them together or apart, it doesn’t matter. But the way you take it may increase or decrease the flushing you may get.
- NAC 500-1000mg twice daily
- Stop taking your statin (in many cases)
- Flax Seeds – 1 cup per day. These may decrease Lp(a)
- CarniteX 2 capsules 2-3 times daily (8-21% reduction in Lp(a))
- Vitamin C: It is important to note that Vitamin C does not significantly decrease the Lp(a) levels. Rather, it protects the artery from the effects of the Lp(a). Think of it as a bullet proof vest for the artery.
- 10,000mg daily (27% decrease). You’ll have to divide this up as it can cause diarrhea. Take it along with D-ribose, Proline 500mg, and Lysine 1000mg (Linus Pauling protocol).
- Vitamin C IV twice weekly
- Berberine 500mg 2-3 times daily. Berberine is a natural PCSK9 inhibitor.
- Gamma delta tocotrienols 200mg at bedtime
- L-Arginine 5 grams per day
- CoQ10 100mg per day
- Omega-3s 5 grams per day
- Sex hormones (estrogen & testosterone). Postmenopausal women have a 30% increased Lp(a)
- Thyroid hormone
- Aspirin 81mg (81% decrease)
- Reduce IL-6 and inflammation
- Exercise
HDL
High-density Lipoprotein (HDL) is an interesting molecule. For years, I thought that this was a major protector against cardiovascular disease. Low levels of HDL seemed to correlate with higher risk of cardiovascular disease. Also, the National Cholesterol Education Program (NCEP) stated that if your HDL was >60 mg/dL then it removed one of your other risk factors for cardiovascular disease. That sounded like a good thing to me.
Over the years, there has been a change in how we think about HDL. HDL has an important, protective function. At least it should. However, it has to be functional. If it isn’t functional then it isn’t protecting you.
Low levels of HDL suggest an increased risk of cardiovascular disease. High levels of HDL may be a red flag that it is non-functional.
When you have your HDL level measured you are actually measuring the balance of what is being produced and what is being cleared. HDL is supposed to bring cholesterol, among other things, back to the liver. High HDL could mean enhanced production of mature HDL (good) or reduced loss of lipid cargo (bad). Low HDL could mean increased loss of cargo (good) or reduced peripheral cholesterol collection (not good).
HDL is involved in Reverse Cholesterol Transport (RCT). This means that HDL picks up cholesterol (among other things) and transports it back to the liver. HDL and ApoA1 levels only account for 40% of Reverse Cholesterol Transport, also known as cholesterol efflux capacity (CEC). The remainder is due to the actual functionality of the HDL as explained above. In fact, there is a 30% increase in CVD for every standard deviation decrease in cholesterol efflux capacity.
Decreases in CEC may help explain the coronary heart disease gap in addition to Lp(a), even when LDL and LDL-P are at goal. HDL levels are strongly associated with the recovery of insulin sensitivity during the acute phase of MI and improves morbidity and mortality.
The target for HDL is: to have good functionality!
How to improve HDL and HDL functionality:
- Niacin
- Omega-3s
- Pantethine
- Red Yeast Rice –
- Mono-Unsaturated Fatty Acids (Olive Oil)
- Lycopene
- Plant sterols
- Glutathione
- Curcumin
- Resveratrol
- Anthrocyanadins
- Flavonoids
- Wogonin (component of Scutellaria baicalensis Georgi extracts)
- Alpha Linolenic Acid (ALA)
- CoQ10
- Phospatidyl Serine
Myeloperoxidase (MPO)
Myeloperoxidase is a marker of inflammation and oxidative stress. It is an enzyme produced by white blood cells that catalyzes the conversion of chloride and hydrogen peroxide to hypochlorite. MPO is primarily anti-infective but it cross reacts with ApoA1 (one of the proteins on the HDL molecule).
MPO inhibits and oxidizes ApoA1 and HDL making them dysfunctional. This reduces HDLs ability to effective transport cholesterol (reverse cholesterol transport).
MPO also oxidizes LDL and promotes foam cells. The video above discusses these foam cells. MPO also degrades the collagen layer which overlays the lipid core in unstable plaque. This makes this plaque more prone to rupture and cause a sudden heart attack.
Elevated MPO levels increase the risk of coronary heart disease 16 fold. That is a 1600% increased risk. Wow! The higher it is and the longer it is high the greater your risk. MPO is supposed to protect you. It is part of the immune system and helps kill infections. However, the continued stimulation starts causing problems.
MPO makes plaques unstable. It contributes to ischemic heart disease & plaques. It consumes and reduces Nitric Oxide (NO) and it contributes to endothelial dysfunction and vasoconstriction. As you can see, MPO is major bad stuff and contributes to inflammation, oxidative stress, and vascular immune dysfunction – the 3 finite responses that cause hypertension and cardiovascular disease.
How to make your HDL functional again:
- Statins
- Niacin – partially reverses the dysfunctional HDL by restoring its anti-inflammatory and anti-oxidative properties.
- Pomegranate – 1/4-1/2 cup (or 6oz of juice) daily
- Quercetin
- EGCG
- Resveratrol
- Glutathione
- Exercise
- Omega-3s
References:
- Am J Cardiol. 2015 Jan 15;115(2):157-60