The idea that HDL cholesterol is cardioprotective is well accepted.
What is not as well appreciated is that, similar to the discordant relationship between the level of LDL‐C and number of low density lipoprotein particles in patients with residual CHD risk, the amount of cholesterol carried within high density lipoprotein particles may also vary significantly between individuals who have the same level of HDL‐C.1,2
For this reason, HDL‐C levels may not be a good indicator of the number of circulating HDL particles present and the amount of cardioprotection they confer.
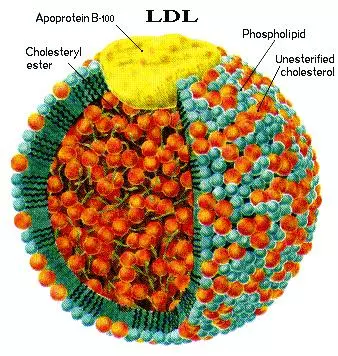
CHD risk is impacted by the interaction of lipoproteins within the arterial wall. Low‐density lipoprotein particles promote atherosclerosis by penetrating the artery wall and subsequently becoming oxidized and ingested by macrophages. These macrophages become cholesterol‐rich foam cells that then deposit their lipid contents into the vessel wall and initiate development of atherosclerotic plaque.
HDL particles antagonize the atherosclerotic process by facilitating reverse cholesterol transport back to the liver, by inhibiting oxidation of LDL and blocking the deposition of lipids into the arterial wall, stimulating vasodilatation, inhibiting platelet aggregation and inhibiting endothelial cell apoptosis.
Therefore, the overall risk of CHD is greatly dependent upon the balance of these atherogenic and anti‐atherogenic processes.2,3
EPIC-Norfolk Study
Dr. Karim El Harchaoui and his colleagues performed a nested case‐control study of 822 apparently healthy men and women within the EPIC‐Norfolk cohort to determine the relationship of HDL particle size and number to risk of future CHD events. They observed that both HDL size and number were independently associated with other CHD risk factors and CHD risk.
Upon correction for metabolic syndrome markers, the HDL size was no longer associated with risk of future CHD events while the relationship of HDL particle number (HDL‐P) to CHD risk was not affected by adjustment for these same parameters. These data suggest that the association of HDL particle size is confounded by metabolic dysregulation, but that HDL‐P is an independent predictor of CHD even after correction for metabolic parameters.4
An earlier publication by Dr. James Otvos and his colleagues report data from a prospective, nested case‐control study of 364 men with a new CHD event to determine if low‐density lipoprotein particle number (LDL‐P) and HDL‐P provide additional information relative to CHD risk reduction at baseline and after 7 months of treatment with gemfibrozil or placebo.
On gemfibrozil treatment, HDL‐C increased by 6% while total HDL‐P increased by 10%. HDL‐C was not a significant predictor of CHD risk either at baseline or on–trial. HDL‐P was a strong, independent predictor of a new CHD event both at baseline and on‐trial. This relationship was preserved even after adjustment for LDL‐C, HDL‐C and triglycerides.5
How To Increase HDL-P
Until work is published containing management guidelines for HDL‐P, physicians are likely to be guided by the National Cholesterol Education Program – ATP III Guidelines that recommend treatment of low HDL‐C (< 40 mg/dL) after LDL‐C goals have been reached and triglycerides are < 200 mg/dL. Intensive weight management and increased physical activity are recommended as well as consideration of prescribing niacin or fibrates to increase HDL‐C.
Conclusion
Multiple studies support the relationship of HDL‐P to CHD outcomes and work continues to address the role HDL‐P plays at the molecular level and to measure the potential benefit of managing to HDL‐P targets. Since cardioprotection is a function of HDL particles themselves and is not a function of the cholesterol carried within them, it is possible that HDL‐P, may be a better indicator of cardioprotection than HDL‐C and may be a suitable target for CVD management.
References
- Cromwell WC, Otvos JD, et al. LDL Particle number and risk of future cardiovascular disease in the Framingham Offspring Study – implications for LDL management. J Clin Lipidol 2007;1:583‐592.
- Cromwell WC. High‐density lipoprotein associations with coronary heart disease: Does measurement of cholesterol content give the best result? J Clin Lipidol 2007;1:57‐64.
- Assmann G, Nofer J. Atheroprotective effects of high‐density lipoproteins. Annu Rev Med 2003;54:321‐41.
- El Harchaoui K, Arsenault BJ, Franssen R. High density lipoprotein particle size and concentration and coronary risk. Ann Intern Med 2009;15084‐93.
- Otvos JD, Collins D, Freedman DS, et al. Low‐density lipoprotein and high‐density lipoprotein particle subclasses predict coronary events and are favorably changed by gemfibrozil therapy in the Veteran’s Affairs High‐Density Lipoprotein Intervention Trial. Circulation 2006;113:1556‐1563.
- ATP III Guidelines At‐A‐Glance Quick Desk Reference. NHLBI. U.S. Department of Health and Human Services, NIH Publication No. 01‐330.
- Cromwell WC, Dayspring T, Richman M. Lipid and Lipoprotein Disorders: Current Clinical Solutions. Pocket Guide. International Guidelines Center. 2009.