Alpha-hydroxybutyrate (α-HB), Linoleoyl-glycerophosphocholine (L-GPC), Oleic Acid, and the IRi Score Test Guide
Test Description
Insulin resistance (IR) plays a fundamental role in the pathogenesis of metabolic syndrome (MetS) and type-2 diabetes mellitus (T2DM).1,2 Insulin Resistance is a continuous variable defined as a decrease in the effectiveness of a given amount of insulin to lower blood glucose levels.
When IR develops in an individual, the pancreatic β cells must produce increased amounts of insulin to control blood glucose. This compensatory response results in the characteristic state of hyperinsulinemia associated with IR, and simultaneously initiates a process of cellular injury and functional decline in the β cells. Eventually, the demand placed on the β cells by insulin resistance exceeds their ability to increase insulin production, and blood glucose levels rise, resulting in prediabetes.
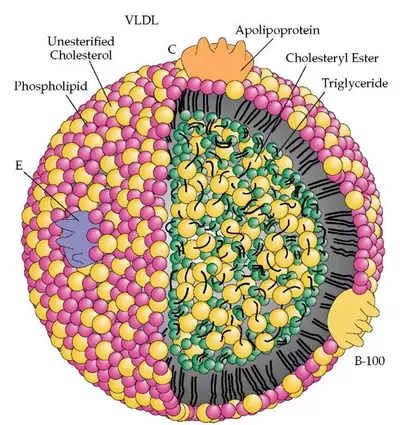
Prediabetes includes impaired fasting glucose (IFG), impaired glucose tolerance (IGT), impaired postprandial glucose (IPG), and combined glucose intolerance (CGI = IFG+IGT or IFG+IPG). Even in the absence of hyperglycemia, IR contributes to the development of cardiovascular disease via effects of hyperinsulinemia on liver lipoprotein metabolism and vascular function.
Insulin Resistance is the earliest detectable metabolic abnormality in individuals at risk for developing T2DM, and may be present decades before hyperglycemia develops (Figure 1).3 Though the rate of progression from Insulin Resistance to frank T2DM varies substantially among individuals, it is well established that the presence of IR in an otherwise healthy individual is a strong predictor of incident T2DM.
Importantly, interventions that reduce IR, such as diet, exercise, or insulin-sensitizing medications like metformin or thiazolidinediones (pioglitazone/Actos®), are also effective in preventing T2DM. Therefore, quantitative measurement of IR is not only useful for detecting risk, but also provides a therapeutic index that provides information about efficacy of different interventions and/or the rate of disease progression in an individual over time.
Because IR typically precedes hyperglycemia by many years and promotes cardiovascular disease independently of hyperglycemia, undiagnosed patients with IR frequently present with advanced cardiovascular disease (CVD) at the time of their initial diagnosis with prediabetes or Type-2 diabetes. Hence, a more rational approach to primary prevention of cardiovascular morbidity and mortality requires earlier diagnosis and intervention, ideally at the point when IR is first detected.
Current diagnostic tests such as blood glucose levels and HbA1c primarily detect prediabetes or diabetes and are severely limited as tools for early detection of insulin resistance. Since hyperglycemia typically does not develop until later stages of the disease process, elevated glucose or A1c occur at a point when interventions may be less effective.4-6 Plasma insulin concentrations are usually elevated in the setting of IR. However, the fasting insulin levels typically measured in clinical settings can vary considerably from day to day in the same individual, limiting their sensitivity and specificity for detecting insulin resistance; in addition, this variability impedes use of fasting insulin levels for monitoring therapeutic responses or the rate of disease progression in an individual patient over time. Moreover, although fasting insulin levels rise in early IR, they can fall again due to β-cell exhaustion in later disease (Figure 1). In contrast, plasma insulin level measured at multiple time-points during a 75 gm, 2 hour oral glucose tolerance test (OGTT) is a powerful tool for both detecting and monitoring IR. However, administering the OGTT with multiple blood draws is beyond the scope of most clinical practices, because it is generally considered too intensive in terms of both time and labor to be used in outpatient settings.
HDL, Inc. is utilizing a patented set of novel small molecule (metabolite) biomarkers to diagnose, quantify, and monitor IR in individual patients over time. These biomarkers were discovered by analyzing the blood of almost 400 insulin-resistant and normal individuals from the RISC (Relationship of Insulin Sensitivity to Cardiovascular Risk) Study, a cohort of clinically characterized nondiabetic individuals,7 to identify several molecules that together present a characteristic pattern of change indicative of insulin resistance (Figure 2). Study subjects were nondiabetic, healthy individuals representing a broad spectrum of insulin sensitivity and glucose tolerance (based on euglycemic-hyperinsulinemic [HI] clamp studies and OGTT).7 485 small molecule metabolites were measured in the blood of each individual by tandem mass spectrometry. This unique metabolomics approach was considered “unbiased” and “hypothesis-free,” because it involved comprehensive measurement of as many endogenous metabolites as possible without any preconceived notions of which ones would be most likely to detect insulin resistance.8 In contrast, traditional disease biomarkers are employed because they are known a priori to relate to some particular aspect of a disease process; as a result, they already correlate with established risk factors for the disease and may therefore provide relatively little additional predictive value.
Of the 485 metabolites screened, alpha-hydroxybutyrate (α-HB) was most significantly associated with IR (measured by the HI clamp) and prediabetes (measured by OGTT).7 A previously unrecognized metabolite, α-HB is an organic acid positioned at the crossroad between amino acid catabolism and glutathione synthesis, just upstream of the tricarboxylic acid (TCA) cycle (Figure 3). It is produced in the liver as a byproduct during the formation of α-ketobutyrate (α-KB), a substrate for cellular energy that is also produced during the formation of the antioxidant glutathione in the setting of hepatic oxidative stress. Therefore, α-HB is elevated in states of increased oxidative stress, increased glutathione demand, impaired mitochondrial energy metabolism, and lipid oxidation, a metabolic feature of IR.9,10 A model has been proposed linking α-HB production to the free fatty acid-rich environment of obesity/insulin resistance—exemplified in the metabolic syndrome and T2DM—with changes in methionine oxidation and glutathione generation, tissue redox balance, and attenuated TCA capacity of insulin- resistant tissues (Figure 3).9,10 In addition, the finding of a positive association between free fatty acid (FFA) levels and plasma α-HB levels in the RISC cohort supports the possibility that an increased NADH/NAD+ ratio favors production of α-HB (Figure 3).7
The next top-ranking biomarker of IR identified by metabolomics was linoleoyl-glycerophosphocholine (L-GPC), a putative lipid-signaling molecule.7 A third high-ranking metabolite, oleic acid was identified. Oleic acid is
a monounsaturated omega-9 fatty acid produced from stearic acid (C18) through the action of stearoyl coA- desaturase (SCD1). In the fasting state, circulating oleic acid levels do not reflect mealtime dietary intake. Oleic acid is the predominant fatty acid of triglycerides normally stored in human adipose tissue, and also those that accumulate in liver in non-alcoholic fatty liver disease (hepatic steatosis).11,12 Since stearic acid is plentiful in most modern diets, increased fasting levels of circulating oleic acid may reflect increased SCD1 activity in fat and liver. Since SCD1 is strongly induced by dietary carbohydrates, elevated oleic acid may specifically reflect end-organ damage from excess carbohydrate-intake—a known risk factor for metabolic syndrome and T2DM—in these tissues.13
Elevated plasma concentrations of α-HB and L-GPC have also been shown to mark for the presence of fatty liver disease independently of sex and age.14 In fact, α-HB may play a direct role in the pathogenesis of IR by inhibiting mitochondrial ATP synthesis in muscle tissue (Metabolon, Inc., personal communication). Evidence also shows that aging is associated with a reduction in plasma L-GPC, and that aerobic exercise can increase plasma L- GPC, along with insulin sensitivity.15
Combining plasma insulin along with α-HB, L-GPC, and oleic acid, generates a composite index for quantifying IR, referred to as “IRi score”. The IRi score provides a more comprehensive assessment of IR than any one metabolite and improves the ability to define where an individual lies on the continuum of diabetes development.16 In comparison to other methods for quantifying IR—including HOMA-IR and the oral glucose sensitivity index derived from OGTT testing—the IRi score exhibits superior correspondence to the gold standard HI clamp measurement of IR.4-6
The three metabolites, α-HB, L-GPC, and oleic acid, are measured at HDL, Inc. by tandem mass spectrometry. Plasma insulin, which is additionally used to calculate the IRi score, is measured by immunoassay. The IRi score is derived as described by Cobb et al.16
Clinical Interpretation
Monitoring changes in fasting plasma α-HB has been shown to alert physicians to early-stage IR and risk for T2DM or CVD. In the initial metabolomics discovery study, levels of α-HB were consistently and significantly higher in the IR subjects with normal glucose tolerance (NGT) compared to normal insulin-sensitive (IS) subjects (p < 0.0001).7 Furthermore, α-HB was able to distinguish insulin-sensitive subjects with NGT (NGT-IS) from insulin-resistant subjects with NGT (NGT-IR), with 76% accuracy, thus providing a highly useful, early indicator of IR. α-HB levels were significantly higher in the NGT-IR, IFG, and IGT groups as compared to the NGT-IS group (p < 0.0001). α-HB concentrations ≥ 5 µg/mL were found to best distinguish NGT-IR from NGT- IS subjects. Individuals in the upper tertile of α -HB concentration (≥ 5.9 µg/mL) were significantly more likely to have both IR (odds ratio 3.26, p < 0.0001) and IGT (odds ratio 2.72, p < 0.0001). Finally, α-HB was also found to separate individuals with NGT from those with prediabetes (IFG or IGT) independently of, and in addition to, IR (odds ratio 2.51, p < 0.0001). Importantly, these associations were independent of sex, age, and BMI. Thus, together with other biomarkers, α-HB provides a diagnostic tool to identify IR with or without prediabetes at an earlier stage of the disease process than currently used clinical tests.7
The second IR biomarker identified from this analysis, L-GPC, significantly decreased in concentration with increasing IR and dysglycemia.7 In a large follow-up study, the predictivity of α-HB and L-GPC for incident dysglycemia was observed in two observational cohorts, comprising 1,048 nondiabetic participants from the RISC study and 2,580 from the Botnia Prospective Study, with 3-year and 9.5-year follow-up data, respectively. In both cohorts, fasting α-HB was positively associated, and L-GPC negatively associated with insulin resistance, independent of other known predictors and independent of one another (p < 0.0001). In addition, α-HB was reciprocally related to indices of β-cell function derived from the oral glucose tolerance test (OGTT; p = 0.0002).17
In the RISC cohort, α-HB levels in the top quartile of its distribution (> 5.48 µg/mL) compared to the bottom quartile conferred a relative risk for IR of 2.84, whereas an L-GPC concentration in the bottom quartile of its distribution (< 11.78 µg/mL) conferred a risk of 3.14. Moreover, in the 122 NGT subjects falling in the highest
α-HB quartile and the lowest L-GPC quartile, the relative risk for IR was 4.14. Changes in α-HB and L-GPC over time tracked with their ability to predict development of prediabetes; after 3 years, α-HB had risen (p = 0.0003) and L-GPC had fallen (p < 0.05) in subjects who progressed to dysglycemia compared with stable NGT subjects. Similar data were obtained in the Botnia study cohort.17 Compared with other selected amino acids and branched- chain amino acids reported to be markers of obesity and insulin resistance and predictive of diabetes,18,19 α-HB and L-GPC were more sensitive markers of IR, e.g., able to discriminate IS from IR individuals in both NGT and IGR ranges.17 Increased α-HB and decreased L-GPC levels thus serve as “readouts of metabolic overload (elevated NADH/NAD+ ratio)” and reduced glucose metabolism in both IR and the earliest phases of prediabetes.17
Follow-up work combined α-HB and L-GPC into an algorithm (the IRi score) developed from an expanded analysis of the RISC cohort.16 This IRi score, based on multiple regression and incorporating α-HB, L-GPC, oleic acid, and fasting insulin, successfully identifies individuals in the lowest tertile of insulin sensitivity (as measured by the HI clamp), with an receiver-operating characteristic area under the curve (ROC-AUC) of 0.79 (p < 0.001).16 The ROC-AUC is a measure of optimal sensitivity and specificity where 1.0 would denote a perfect study with 100% positive predictive value and 100% negative predictive value. Remarkably, the IRi score was also statistically equivalent to the HI clamp itself in predicting conversion from NGT to IGT in a 3-year follow-up of the RISC subjects (ROC-AUC = 0.70, n = 899).16 In a cross-sectional analysis of 543 individuals from the Botnia
Prospective Study, the algorithm was measured and compared in those who progressed to T2DM versus those who did not.17 Over a 3-year period, the top-ranking insulin sensitivity metabolites, α-HB and L-GPC alone, predicted progression to T2DM with AUCs of 0.73 (p < 0.005) and 0.69 (p < 0.05), whereas the IRi algorithm exhibited an ROC-AUC of 0.80 (p = 0.00002).20
In summary, these insulin sensitivity markers—α-HB, L-GPC, oleic acid, and the associated IRi score— measured in a fasting plasma sample, can identify high-risk, insulin-resistant subjects with very high accuracy early in the disease process, and provide an early indication of risk for progression to prediabetes and T2DM.
Treatment Considerations
α-HB alone, and combined with L-GPC, oleic acid, and insulin in the IRi score, acts as a highly sensitive biomarker of early insulin resistance and progression toward prediabetes, even in normoglycemic individuals. Together with other biochemical and clinical parameters these metabolites can accurately detect subclinical abnormalities of glucose metabolism. The IRi score demonstrates expected improvement upon successful treatment with pharmacological insulin-sensitizer therapies.21
By identifying individuals at significantly increased risk for prediabetes and diabetes, appropriate dietary, lifestyle, and perhaps pharmaceutical interventions can be implemented to prevent/reverse disease progression. The IRi score may subsequently be useful for tracking the restoration of insulin sensitivity associated with improvements in patients’ glycemic status.
In summary:
The IRi score and its constituent metabolites fill a gap in clinical care for earlier detection of high-risk IR patients and dysglycemia. Each of the 4 analytes contributes complementary and unique information from different metabolic pathways related to insulin function.
This is a practical, fasting metabolic test for improved detection and management of high-risk, dysmetabolic IR patients and for quantifying the risk of progression to T2DM.
- Simple measurement from fasting blood of analytes α-HB, L-GPC, and oleic acid allow the physician to identify patients with IR in its earliest stages as well as monitor the effectiveness of anti-diabetes therapies.
- Pioglitazone modulates these 3 analytes by reducing plasma α-HB and oleic acid and increasing
L-GPC concentrations, in proportion to improvement in insulin sensitivity.21 The IRi score can thus be used to track improvement in ACTOS®-treated prediabetics.
- The IRi score has strong clinical data validating its correlation with the euglycemic hyperinsulinemic clamp, the gold standard for measuring IR.
- α-HB and the IRi score may improve patient care and compliance with lifestyle and/or medication adherence, thereby, more effectively preventing or delaying disease and IR complications in diabetes and CVD.
- α-HB and the IRi score will enhance CVD risk and glycemic diagnostic panels by allowing physicians to measure IR directly and assess cardiometabolic risk more sensitively and accurately.
NOTE: Other factors may contribute to elevated serum and/or urinary α-HB levels, via increases in the NADH/NAD+ ratio associated with lipid oxidation or increased glutathione demand due to oxidative stress. These may include heavy alcohol consumption, smoking, poor diet, and acute viral infections.10,22,23
If FPG and HbA1c are abnormal, follow therapeutic guidelines of the American Diabetes Association. The following lifestyle recommendations and medications can be used to reduce insulin resistance and improve β-cell function, personalized to the individual patient’s clinical needs.
Lifestyle24-30:
- Limit carbohydrates (especially simple sugars and processed carbohydrates) while maintaining moderate fat intake
- Weight loss (as appropriate)
- Regular exercise (150 minutes/week combining cardiovascular activity at a moderate-to-vigorous pace with resistance training)
Medication choices may include:
- Metformin (e.g., Glucophage®, Glumetza®)
- Pioglitazone (Actos®)
- Incretin mimetics (GLP-1 agonists)
- DPP-4 inhibitors
- Quick-release bromocriptine mesylate (Cycloset®)
- Alpha-glucosidase inhibitors (acarbose)
NOTE: No medications are currently FDA approved for the treatment of insulin resistance or β-cell dysfunction. Insulin may be considered for the treatment of hyperglycemia meeting ADA criteria for diabetes but should NOT be used in the setting of insulin resistance without diabetes or in prediabetes due to the potential for hypoglycemia.31 Patients who are taking metformin are at increased risk for vitamin B12 deficiency and may benefit from sublingual vitamin B12 supplementation.32
References
- DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 1991;14(3):173-94.
- Duvnjak L, Duvnjak M. The metabolic syndrome – an ongoing story. J Physiol Pharmacol 2009;60 Suppl 7:19-24.
- Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58(4):773-95.
- Borai A, Livingstone C, et al. Selection of the appropriate method for the assessment of insulin resistance. BMC Med Res Methodol 2011;11:158.
- Herder C, Karakas M, et al. Biomarkers for the prediction of type 2 diabetes and cardiovascular disease. Clin Pharmacol Ther 2011;90(1):52-66.
- Goldfine AB, Gerwien RW, et al. Biomarkers in fasting serum to estimate glucose tolerance, insulin sensitivity, and insulin secretion. Clin Chem 2011;57(2):326-37.
- Gall WE, Beebe K, et al. alpha-hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS ONE 2010;5(5):e10883.
- Suhre K, Meisinger C, et al. Metabolic footprint of diabetes: a multiplatform metabolomics study in an epidemiological setting. PLoS ONE 2010;5(11):e13953.
- Adams SH. Emerging perspectives on essential amino acid metabolism in obesity and the insulin-resistant state. Adv Nutr 2011;2(6):445-56.
- Lord RS, Bralley JA. Clinical applications of urinary organic acids. Part I: Detoxification markers. Altern Med Rev 2008;13(3):205-15.
- Hodson L, Fielding BA. Stearoyl-CoA desaturase: rogue or innocent bystander? Prog Lipid Res 2013;52(1):15-42.
- Ntambi JM, Miyazaki M. Recent insights into stearoyl-CoA desaturase-1. Curr Opin Lipidol 2003;14(3):255-61.
- Wolever TM, Mehling C. Long-term effect of varying the source or amount of dietary carbohydrate on postprandial plasma glucose, insulin, triacylglycerol, and free fatty acid concentrations in subjects with impaired glucose tolerance. Am J Clin Nutr 2003;77(3):612-21.
- Gastaldelli A, Natali A, et al. α-hydroxybutyrate and linoleoyl-glycerolphosphocholine as new markers of fatty liver disease [abstract]. Diabetes 2011;60(Suppl 1):A453.
- Garcia J, Lum H, et al. Effect of aging and exercise on novel insulin sensitivity marker linoleoyl-glycerophosphocholine [abstract]. Diabetes 2012;61(Suppl 1):A181.
- Cobb J, Gall W, et al. A novel fasting blood test for insulin resistance and prediabetes. J Diabetes Sci Technol 2013;7(1):100-10.
- Ferrannini E, Natali A, et al. Early metabolic markers of the development of dysglycemia and type 2 diabetes and their physiological significance. Diabetes 2013;62(5):1730-7.
- Newgard CB. Interplay between lipids and branched-chain amino acids in development of insulin resistance. Cell Metab 2012;15(5):606-14.
- Wurtz P, Makinen VP, et al. Metabolic signatures of insulin resistance in 7,098 young adults. Diabetes 2012;61(6):1372-80.
- Gall W, Mitchell MW, et al. Metabolic markers of insulin sensitivity predict progression to IGT and T2D [abstract]. Diabetes Metab 2011;60(Suppl 1):A414.
- Tripathy D, Gall W, et al. Pioglitazone improves insulin sensitivity by modulating novel biomarkers: results from the ACTNOW study [abstract]. Diabetologia 2011;54(Suppl 1):S30.
22. Imaki M, Kawabata K, et al. Evaluation of the effects of various factors on the serum alpha hydroxybutyrate dehydrogenase activity in
young females. Appl Human Sci 1995;14(6):297-302.
23. Silva AR, Ruschel C, et al. Inhibition of in vitro CO2 production and lipid synthesis by 2-hydroxybutyric acid in rat brain. Braz J Med Biol
Res 2001;34(5):627-31.
24. Mirza NM, Palmer MG, et al. Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American
children and adolescents: a randomized controlled trial. Am J Clin Nutr 2013;97(2):276-85.
25. Yki-Jarvinen H. Nutritional modulation of nonalcoholic fatty liver disease and insulin resistance: human data. Curr Opin Clin Nutr Metab
Care 2010;13(6):709-14.
26. Bradley U, Spence M, et al. Low-fat versus low-carbohydrate weight reduction diets: effects on weight loss, insulin resistance, and
cardiovascular risk: a randomized control trial. Diabetes 2009;58(12):2741-8.
27. Ross R, Janssen I, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res
2004;12(5):789-98.
28. O’Hagan C, De Vito G, et al. Exercise prescription in the treatment of type 2 diabetes mellitus : current practices, existing guidelines and
future directions. Sports Med 2013;43(1):39-49.
29. Davidson LE, Hudson R, et al. Effects of exercise modality on insulin resistance and functional limitation in older adults: a randomized
controlled trial. Arch Intern Med 2009;169(2):122-31.
30. Williams MA, Haskell WL, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific
statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and
Metabolism. Circulation 2007;116(5):572-84.
31. Aguilar RB. Evaluating treatment algorithms for the management of patients with type 2 diabetes mellitus: a perspective on the definition
of treatment success. Clin Ther 2011;33(4):408-24.
32. Moore EM, Mander AG, et al. Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes
Care 2013;36(10):2981-7.