Insulin Resistance Labs – Leptin
History of Leptin
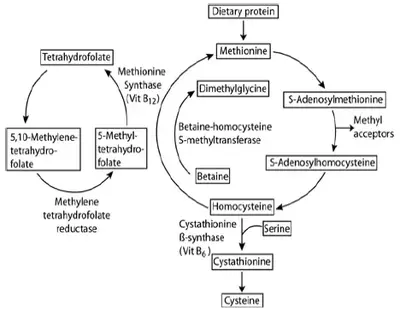
Leptin was discovered in 1994 when Friedman and colleagues performed positional cloning of the ob gene, responsible for a recessive mutation found decades earlier to cause obesity in the homozygous ob /ob mouse.1 The researchers discovered that this gene encodes a secreted peptide hormone, expressed almost exclusively in adipose tissue, which they named “leptin.”
Deficiency of leptin in the homozygous ob /ob mice causes morbid obesity, severe insulin resistance, hyperglycemia, hyperphagia (uncontrolled eating behavior), decreased energy expenditure, lethargy, central hypothyroidism, and other neuroendocrine abnormalities.1,2 Treatment of ob /ob mice with purified leptin reduces food intake, normalizes insulin-glucose homeostasis, increases energy expenditure, and reduces body weight.3,4
Leptin acts primarily on the hypothalamus to induce metabolic changes in brown adipose tissue and skeletal muscle via the sympathetic nervous system; specifically, leptin enhances mitochondrial function and induces the mitochondrial uncoupling protein UCP1 in these tissues, producing an enormous increase in energy expenditure via thermogenesis (body heat production).5 Because lipids (fatty acids in particular) are the primary fuel substrate for mitochondrial thermogenesis, leptin treatment also reverses the pathological accumulation of lipid (i.e., lipotoxicity) that causes insulin resistance and glucose intolerance in ob /ob mice.6 The net effect of these changes is rapid weight reduction and normalization of insulin-glucose homeostasis in leptin-treated ob /ob mice.3
Identification of the human leptin gene (OB or LEP ) in 1995 opened the possibility of using leptin to treat human obesity, insulin resistance, and diabetes.7 This possibility was confirmed in part with the discovery of individuals with recessive loss-of-function mutations in the human leptin gene. These mutations are extremely rare, with only a handful of affected families discovered worldwide in the past decade.8 Analogous to the ob/ob mice, a leptin deficient individual has no detectable circulating leptin and is obese, hyperphagic, and severely insulin-resistant from early childhood. Treatment with recombinant human leptin reverses all of these defects and normalizes metabolism in these individuals in a matter of weeks.9
Leptin has also been found to be effective in reducing metabolic abnormalities in individuals who lack normal adipose tissue depots due to congenital or acquired generalized lipodystrophies.10,11 Unlike individuals with genetic leptin deficiency, lipodystrophic individuals are exceedingly lean and produce little or no leptin due to the lack normal adipose tissue (where leptin is normally produced).12 Lipodystrophic individuals adapt to the inability to store lipids in fat by inappropriately storing them in other tissues such as muscle and liver, resulting in severe lipotoxic insulin resistance, diabetes, and eventually fulminant liver failure due to steatohepatitis.13 Leptin treatment of lipodystrophic individuals reverses or ameliorates these metabolic derangements.
Despite these examples of beneficial effects of leptin treatment, studies with purified recombinant human leptin in common types of obesity were disappointing: most individuals with obesity exhibit little or no change in weight with leptin treatment.14,15 Why is this?
Leptin regulates feeding behavior and metabolism
The brain (hypothalamus) receives information from “adiposity signals” such as the hormones insulin and leptin (reflecting long-term energy availability) and signals from nutrients such as glucose and free fatty acids (reflecting short-term energy availability).16,17
When there is sufficient access to food and body fat stores are ample, feeding behavior and metabolism should be adjusted to decrease energy intake (enhance the sense of satiety) and endogenous glucose production, while simultaneously increasing energy expenditure and mobilizing fat stores.18
On the other hand, if the brain has decreased signal input from these “adiposity signals” then the brain adjusts metabolism to increase nutrients in the blood stream. In part, this is accomplished by increasing glucose production (gluconeogenesis) in the liver.19 With the consequent rise in body fat content and blood glucose levels, blood levels of leptin, insulin, and free fatty acids also increase, providing negative feedback to the brain and restoring food intake and glucose production to their former values.15
Leptin production is directly coupled to fat mass, obese people generally exhibit unusually high circulating levels of leptin that are sustained over many years. This chronic elevation of leptin in obesity, along with hyperinsulinemia and other metabolic derangements, are believed to produce a state of “leptin resistance” in the hypothalamus.16 In effect, the primary pathway through which leptin controls appetite and metabolism becomes inherently flawed at some point in obese individuals, such that the brain does not adequately receive or relay the signal to decrease food intake and increase energy expenditure.
Leptin:BMI Ratio
It is now recognized that leptin resistance may be variable among obese individuals. Calculation of the plasma leptin:body mass index (BMI) ratio (i.e., a “BMI-adjusted” leptin level) is one way to quantify severity of leptin resistance in obese individuals.20
Leptin:BMI ratios vary substantially among obese individuals, because circulating leptin levels reflect both total adipose tissue mass (estimated by BMI) and the severity of hypothalamic leptin resistance. Sympathetic enervation of adipose tissue and circulating catecholamines normally suppress production and release of leptin by adipose tissue.21,22
Leptin resistance in the hypothalamus and the subsequent decreased sympathetic outflow to fat produces even greater production and release of leptin (further aggravating hypothalamic leptin resistance in a feed-forward manner). Therefore, if circulating leptin levels are in excess to fat mass (estimated by BMI), it is indicative of a more severe state of leptin resistance. The leptin:BMI ratio provides a quantitative assessment for the severity of leptin resistance in obesity.
For the same age and BMI, women have significantly higher leptin concentrations than men (mean levels: women 14.13 pg/mL vs. men 5.73 pg/mL).23
Leptin risk ranges are:
- High risk: > 43 ng/mL
- Intermediate risk: 20–43 ng/mL
- Optimal: < 20 ng/mL
The risk ranges for the Leptin:BMI ratio are:
- High-risk: > 1.17
- Intermediate risk: 0.66–1.17
- Optimal: < 0.66
Clinical Interpretation
While absolute leptin deficiency causes obesity, most obese individuals exhibit elevated circulating plasma leptin levels—as would be expected, given that leptin is synthesized and secreted by adipocytes in direct proportion to total body fat mass.16
Leptin resistance
Sustained elevations in plasma leptin levels are associated with obesity, overeating, and inflammation-related diseases including hypertension, metabolic syndrome, and cardiovascular disease (CVD).24 It is thought that increases in leptin level (in response to caloric intake) act as an acute response mechanism to prevent excess cellular stress caused by over-eating when adipose tissue depots are already replete, which can lead to ectopic fat storage within internal organs, arteries, and muscle.25 In other words, Leptin is trying to keep you from over-eating.
The postprandial rise in circulating insulin levels induces an increase in leptin in a dose-dependent fashion. This effect is enhanced by high cortisol levels.26 However, although most obese individuals have high leptin levels, these common forms of obesity are associated with acquired impairment in the response to elevated leptin levels, which therefore do not induce the expected reduction in feeding and body weight that would mitigate obesity.
Furthermore, although recombinant leptin can be used to treat the rare monogenic form of leptin deficiency and the generalized lipodystrophies, administering the hormone to obese individuals does not always induce weight loss as predicted, suggesting that they may be resistant to the effects of leptin.27
Such “leptin resistance” is thought to be an important component in the development of obesity and is somewhat analogous to “insulin resistance,” wherein elevated insulin levels are required to maintain blood glucose levels in the normal range.27,28 The chronic hyperleptinemia which characterizes obesity decreases the transport of leptin into the central nervous system (CNS) and/or impairs the signaling properties of leptin receptors such that acute leptin responses do not adequately signal “fullness” to the brain to curb hunger.
This confers increased susceptibility to diet-induced obesity, which in turn raises leptin levels further and worsens leptin resistance, leading to a vicious cycle of weight gain. Therefore in addition to being a major cause of obesity, leptin resistance is also an important consequence.28-30
Leptin controls feeding not just by providing a physiological satiety signal, but also by modulating the perception of reward associated with feeding.30 This action of leptin probably occurs at the level of the mesolimbic dopaminergic system, and may explain the weight gain commonly induced by antipsychotic drugs, which act as mixed dopamine receptor antagonists.31
Based on existing knowledge, obese individuals with more severe leptin resistance are likely to struggle more with dieting and weight loss through lifestyle interventions and may experience rebound of weight gain more quickly after weight loss; in addition, these individuals may exhibit more severe insulin resistance along with an increased number and severity of components of the metabolic syndrome (e.g., hyperglycemia, central adiposity, hypertension, hypertriglyceridemia, and reduced HDL-cholesterol).17
Since production of adiponectin by adipose tissue is generally suppressed by worsening insulin resistance, the leptin:adiponectin ratio may be useful in assessing the synergistic metabolic impairment caused by insulin resistance and leptin resistance in a given individual. Consistent with this, several recent studies have demonstrated that the leptin:adiponectin ratio is a novel, independent predictor of type 2 diabetes (T2DM) and CVD.32-35
Leptin affects glucose metabolism and insulin sensitivity in peripheral tissues
Outside of the Central Nervous System, leptin can directly affect glucose metabolism by enhancing insulin action in the skeletal muscle, liver, adipose tissue, and by improving function of the pancreatic β cells.36 Leptin suppresses insulin secretion from the pancreas, decreases the production of glucose in the liver, and increases glucose and fatty acid oxidation in both muscle and adipose tissue.36,37 Most of the effects of leptin are mediated on these tissues indirectly via leptin actions in the hypothalamus.
Consistent with this, epidemiologic data show a strong association between insulin resistance and the chronically increased leptin levels associated with leptin resistance (reviewed in 38). The hyperinsulinemia ensuing from insulin resistance plus loss of the protective effects of leptin action can augment the exhaustion and apoptosis of pancreatic β cells, eventually resulting in T2DM.39,40 Pancreatic β cells have leptin receptors and leptin may also be an important direct regulator of β-cell function at different levels including insulin gene expression, insulin secretion, cell growth, and apoptosis.36,38
Although leptin treatment reduces insulin levels and enhances insulin sensitivity in various hypoleptinemic states (primarily by decreasing body weight and fat mass),41 it does not improve insulin sensitivity in obese individuals or those with T2DM for whom leptin excess is associated with leptin resistance.38,42
Leptin and inflammation
A link exists between obesity and chronic inflammation, and it has been proposed that leptin regulates some aspects of the inflammatory response. Leptin production is acutely increased during infection and inflammation.43,44 Elevated leptin also affects the hypothalamic-pituitary-adrenal (HPA) axis and is associated with raised white blood cell counts, indicating a role in the physiological stress response.45,46
Factors that influence inflammatory markers in general can acutely affect leptin levels. In such situations leptin may no longer strictly correlate with body fat mass:43,44
- Leptin levels decrease after short-term fasting (24–72 hour), even when body fat mass does not.47
- Leptin levels are elevated in obese patients with obstructive sleep apnea, but decrease after CPAP treatment.48
- Sleep deprivation reduces leptin levels (leptin is released into the circulation in a pulsatile fashion, following a circadian rhythm, and hence is affected by sleep patterns).49,50 However, sleep disturbances have been shown to increase leptin levels in women of normal weight who have depressed mood.51
- Chronic exercise training decreases leptin levels.52
- Perceived emotional stress reduces leptin levels.53
- Leptin levels are decreased by testosterone and increased by estrogen.54
- Renal failure results in higher leptin levels.55 Leptin levels may be higher in women at the luteal phase of the menstrual cycle, and menopause is associated with a decline in circulating leptin.56,57
Leptin and cardiovascular disease
The relationship between leptin and CVD is complex.58-60 Leptin is necessary for normal cardiac function, as it plays a critical role in preventing cardiac lipotoxicity (lipid accumulation) in obesity.61
In animal models of leptin deficiency, leptin treatment also reduces cellular damage via suppression of cardiomyocyte apoptosis in animal models of ischemia reperfusion injury.62 However, leptin deficiency in animals is distinctly different from the phenomena of leptin resistance and hyperleptinemia that typify normal human obesity.
Hyperleptinemia is present in patients with coronary heart disease, chronic heart failure, hypertension, stroke, and in those at increased risk of myocardial infarction (MI).42,58,59,63 Hyperleptinemia may play a direct role in the pathogenesis of CVD by inducting platelet activation, smooth muscle cell proliferation, endothelial dysfunction, and oxidative stress.64
Consistent with these pro-atherogenic effects, elevated plasma leptin concentrations are independently associated with carotid intimal-medial thickness (CIMT) and with coronary artery calcification score in patients with T2DM, even after controlling for adiposity.60
These pro-atherogenic effects of leptin have obvious negative implications for obese individuals exhibiting leptin resistance. Nevertheless, the complex association between leptin and cardiac function may be one factor underlying the so-called “obesity paradox”; i.e., the observation that survival from certain CVD-related endpoints may be paradoxically increased in individuals with increased BMI.”65
Treatment
To date, several interventional studies have been performed to evaluate the effects and safety of leptin administration in lipoatrophic or obese patients with hypoleptinemia. Administering recombinant human leptin can reverse the obesity of leptin-deficient (but NOT leptin-resistant) individuals and corrects many of the associated metabolic abnormalities including diabetes, dyslipidemia, and hepatic steatosis.66-68
Clinical trials are ongoing to find a modified, more potent therapeutic with a longer half-life, to reduce the frequency of injections and accompanying skin inflammation.69-71 Leptin replacement to children with congenital leptin deficiency remarkably ameliorates hyperinsulinemia and hyperlipidemia.72 Recent randomized trials demonstrate that combination treatment with an amylin analog and human recombinant leptin significantly decreases not only body weight but also insulin levels in obese subjects.73
Importantly, individuals with evidence of more severe leptin resistance will likely require greater medical and social support measures to achieve and maintain substantial weight loss through lifestyle modifications such as diet and exercise. Hence, these individuals may benefit from more frequent and intensive interaction with medical providers, dieticians, and nutrition and exercise counselors to successfully lose weight and maintain weight loss.
In addition, bariatric surgery may be a consideration in the treatment of obese individuals with leptin resistance, especially for individuals with type 2 diabetes or other obesity-related morbidities recognized as indications for bariatric surgery.
In general, for obese individuals with elevated circulating leptin levels, weight loss may be one of the primary therapeutic targets. The following lifestyle recommendations and medications can be used to reduce insulin resistance and improve β-cell function, personalized to the individual patient’s clinical needs.
Lifestyle74-80 :
- Limit carbohydrates (especially simple sugars and processed carbohydrates) while maintaining moderate fat intake
- Weight loss (as appropriate)
- Regular exercise (150 minutes/week combining cardiovascular activity at a moderate-to-vigorous pace with resistance training)
Medication choices may include:
- Metformin (e.g., Glucophage®, Glumetza®)
- Pioglitazone (Actos®)
- Incretin mimetics (GLP-1 agonists)
- DPP-4 inhibitors
- Quick-release bromocriptine mesylate (Cycloset®)
- Alpha-glucosidase inhibitors (acarbose)
- Leptin Manager (supplement from Xymogen) – shown to reduce weight (0.55kg loss in 12 wks) and leptin levels.
References
Zhang Y, Proenca R, Maffei M, et al. Positional cloning of the mouse obese gene and its human homologue. Nature 1994;372(6505):425-432.
Frederich RC, Hamann A, Anderson S, et al. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med 1995;1(12):1311-1314.
Pelleymounter MA, et al. Effects of the obese gene product on body weight regulation in ob/ob mice. Science 1995;269(5223):540-543.
Halaas JL, et al. Weight-reducing effects of the plasma protein encoded by the obese gene. Science 1995;269(5223):543-546.
Cannon B, Nedrgaard J. Brown adipose tissue: function and physiological significance. Physiol Rev 2004;84: 277-359.
Unger RH, Scherer PE. Gluttony, sloth and the metabolic syndrome: a roadmap to lipotoxicity. Trends Endocrinol Metab 2010;21(6):345-52.
Green ED, Maffei M, Braden VV, et al. The human obese (OB) gene: RNA expression pattern and mapping on the physical, cytogenetic, and genetic maps of chromosome 7. Genome Res 1995;5(1):5-12.
El-Sayed Moustafa JS, Froguel P. From obesity genetics to the future of personalized obesity therapy. Nat Rev Endocrinol 2013 9(7):402-13.
Farooqi IS, Matarese G, Lord GM, et al. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest 2002;110:1093-103.
Oral EA, Simha V, Ruiz E, et al. Leptin-replacement therapy for lipodystrophy. N Engl J Med 2002;346(8):570-8.
Chan JL, Lutz K, Cochran E, et al. Clinical effects of long-term metreleptin treatment in patients with lipodystrophy. Endocr Pract 2011;17(6):922-32.
Firoenza CG, Chou SH, Mantzoros CS. Lipodystrophy: pathophysiology and advances in treatment. Nat Rev Endocrinol 2011;7(3):137-150.
Capeau J, Magré J, Lascols O, et al. Diseases of adipose tissue: genetic and acquired lipodystrophies. Biochem Soc Trans 2005;33(5):1073-7.
Zelissen PM, Stenlof K, Lean ME, et al. Effect of three treatment schedules of recombinant methionyl human leptin on body weight in obese adults: a randomized, placebo-controlled trial. Diabetes Obes Metab 2005;7(6):755-61.
Heymsfield SB, Greenberg AS, Fujioka K, et al. Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA 1999;282(16):1568-75.
Schwartz MW, Porte D Jr. Diabetes, obesity, and the brain. Science 2005;307:375-379.
Lustig RH. Childhood obesity: behavioral aberration or biochemical drive? Reinterpreting the First Law of Thermodynamics. Nat Clin Pract Endocrinol Metab 2006;2(8):447-58.
Obici S, Rossetti L. Minireview: nutrient sensing and the regulation of insulin action and energy balance. Endocrinology 2003;144(12):5172-8.
Ahima RS, et al. Role of leptin in the neuroendocrine response to fasting. Nature 1996;382(6588):250-252.
Shah NR, Braverman ER. Measuring adiposity in patients: the utility of body mass index (BMI), percent body fat, and leptin. PLoS One 2012;7(4):e33308.
Ricci MR, Fried SK. Isoproterenol decreases leptin expression in adipose tissue of obese humans. Obes Res 1999;7(3):233-40.
Ricci MR, Lee MJ, Russell CD, et al. Isoproterenol decreases leptin release from rat and human adipose tissue through posttranscriptional mechanisms. Am J Physiol Endocrinol Metab 2005;288(4):E798-804.
Fulda S, Linseisen J, Wolfram G, et al. Leptin plasma levels in the general population: influence of age, gender, body weight and medicalb history. Protein Pept Lett 2010;17(11):1436-40.
Gautron L, Elmquist JK. Sixteen years and counting: an update on leptin in energy balance. J Clin Invest 2011;121(6):2087-2093.
Morton JM, Schwartz MW. Leptin and the central nervous system control of glucose metabolism. Physiol Rev 2011;91:380-411.
Wabitsch M, Jensen PB, Blum WF, et al. Insulin and cortisol promote leptin production in cultured human fat cells. Diabetes 1996;45(10):1435–1438.
Scarpace PJ, Zhang Y. Leptin resistance: a prediposing factor for diet-induced obesity. Am J Physiol Regul Integr Comp Physiol 2009;296:R493–R500.
Martin SS, Qasim A, Reilly MP. Leptin resistance. A possible interface of inflammation and metabolism in obesity-related cardiovascular disease. JACC 2008;52(15):1201-1210.
Mantzoros CS, Magkos F, Brinkoetter M, et al. Leptin in human physiology and pathophysiology. Am J Physiol Endocrinol Metab 2011;301:E567-E584.
Oswal A, Giles Y. Leptin and the control of body weight: A review of its diverse central targets, signaling mechanisms, and role in the pathogenesis of obesity. Obesity 2010;18:221-229.
Bergman RN, Ader M. Atypical antipsychotics and glucose homeostasis. J Clin Psychiatry 2005;66:504-514.
Zaletel J, Barlovic DP, Prezelj J. Adiponectin-leptin ratio: a useful estimate of insulin resistance in patients with Type 2 diabetes. J Endocrinol Invest 2010;33(8):514e8.
Oda N, Imamura S, Fujita T, et al. The ratio of leptin to adiponectin can be used as an index of insulin resistance. Metabolism 2008;57(2):268e73.
Rasmussen-Torvik LJ, Wassel CL, Ding J, et al. Associations of body mass index and insulin resistance with leptin, adiponectin, and the leptin-to-adiponectin ratio across ethnic groups: the Multi-Ethnic Study of Atherosclerosis (MESA). Ann Epidemiol 2012;22(10):705-9.
Kappelle PJ, Dullaart RP, van Beek AP, et al. The plasma leptin/adiponectin ratio predicts first cardiovascular event in men: a prospective nested case-control study. Eur J Intern Med 2012;23(8):755-9.
Marroqui L, Gonzalez A, Neco P, et al. Role of leptin in the pancreatic β-cell: effects and signaling pathways. J Molec Endocrinol 2012;49:R9-R17.
Minokoshi Y, Kim YB, Peroni OD, et al. Leptin stimulates fatty acid oxidation by activating AMP-activating protein kinase. Nature 2002;415:339-343.
Lee YH, Magkos F, et al. Effects of leptin and adiponectin on pancreatic β-cell function. Metabolism 2011;60:1664-1672.
Kieffer TJ, Habener JF. The adipoinsular axis: effects of leptin on pancreatic beta-cells. Am J Physiol Endocrinol Metab 2000;278:E1-4.
Seufert J. Leptin effects on pancreatic beta-cell gene expression and function. Diabetes 2004;53(Suppl 1):S152-8.
Dardeno TA, Chou SH, Moon HS, et al. Leptin in human physiology and therapeutics. Front Neuroendocrinol 2010;31:377-393.
Ren J. Leptin and hyperleptinemia – from friend to foe for cardiovascular function. J Endocrinol 2004;181(1):1-10.
Fantuzzi G, Faggioni R. Leptin in the regulation of immunity, inflammation, and hematopoiesis. J Leukoc Biol 2000;68(4): 437–46.
Matarese G, Procaccini C, De Rosa V, et al. Regulatory T cells in obesity: the leptin connection. Trends Mol Med 2010;16(6):247-56.
Heiman ML, Ahima RS, Craft LS, et al. Leptin inhibition of the hypothalamic-pituitary-adrenal axis in response to stress. Endocrinology 1997;138(9):3859–3863.
Mabuchi T, Yatsuya H, Tamakoshi K. Association between serum leptin concentration and white blood cell count in middle-aged Japanese men and women. Diabetes Metab Res Rev 2005;21(5):441–447.
Chan JL, Heist K, DePaoli AM, Veldhuis JD, Mantzoros CS. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest 2003;111(9):1409–1421.
Harsch IA, Konturek PC, Koebnick C, et al. Leptin and ghrelin levels in patients with obstructive sleep apnoea: effect of CPAP treatment. Eur Respir J 2003;22(2): 251–257.
Seaborg E. Growing evidence links too little sleep to obesity and diabetes. Endocrine News 2007: 14–15.
Knutson KL, Spiegel K, Penev P, et al. The metabolic consequences of sleep deprivation. Sleep Med Rev 2007;11(3):163–178.
Hafner S, Baumert J, Lacriz ME, et al. Sleep disturbances and depressed mood: a harmful combination associated with increased leptin levels in women with normal weight. Biol Psychol 2012; 89(1):163-9.
de Salles BF, Simão R, Fleck SJ, et al. Effects of resistance training on cytokines. Int J Sports Med 2010;31(7):441–450.
Otsuka R, Yatsuya H, Tamakoshi K, et al. Perceived psychological stress and serum leptin concentrations in Japanese men. Obesity (Silver Spring) 2006;14(10):1832–1838.
Ahima RS, Flier JS. Leptin. Annu Rev Physiol 2000;62:413–437.
Mantzuros CS. Leptin in renal failure. J Ren Nutr 1999;9:122-125.
Asimakopoulos B, Milousis A, Gioka T, et al. Serum pattern of circulating adipokines throughout the physiological menstrual cycle. Endocr J 2009;56(3):425-33.
Ben Ali S, Jemaa R, Ftouhi B, et al. Relationship of plasma leptin and adiponectin concentrations with menopausal status in Tunisian women. Cytokine 2011;56(2):338-42.
Sweeney G. Cardiovascular effects of leptin. Nat Rev Cardiol 2010;7:22-29.
Abel ED, Sweeney G. Modulation of the cardiovascular system by leptin. Biochimie 2012;94:2097-2103.
Reilly MP, Iqbal N, Schutta M, et al. Plasma leptin levels are associated with coronary atherosclerosis in type 2 diabetes. J Clin Endocrinol Metab 2004;89(8):3872-8.
Lee Y, Naseem RH, Duplomb L, et al. Hyperleptinemia prevents lipotoxic cardiomyopathy in acyl CoA synthase transgenic mice. Proc Natl Acad Sci USA 2004;101(37):13624-9.
Smith CC, Yellon DM. Adipocytokines, cardiovascular pathophysiology and myocardial protection. Pharmacol Ther 2011;129(2):206-19.
Söderberg S, Ahrén B, Jansson JH, et al. Leptin is associated with increased risk of myocardial infarction. J Intern Med 1999;246(4):409-18.
Beltowski J. Leptin and atherosclerosis. Atherosclerosis 2006;189(1):47-60
Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 2009;53:1925-32.
Oral EA, et al. Leptin-replacement therapy for lipodystrophy. N Engl J Med 2002;346(8):570-578.
Licinio J, et al. Phenotypic effects of leptin replacement on morbid obesity, diabetes mellitus, hypogonadism, and behavior in leptindeficient adults. Proc Natl Acad Sci USA 2004;101(13)4531-4536.
Kelesidis T, Kelesidis I, Chou S, et al. Narrative review: the role of leptin in human physiology: emerging clinical applications. Ann Intern Med 2010;152:93-100.
Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature 1998;395(6704):763–770.
Heymsfield SB, Greenberg AS, Fujioka K, et al. Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA 1999;282(16):1568–1575.
Lo KM, Zhang J, Sun Y, et al. Engineering a pharmacologically superior form of leptin for the treatment of obesity. Protein Eng Des Sel 2005;18(1):1–10.
Farooqi IS, Matarese G, Lord GM, et al. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest 2002;110:1093-103.
Ravussin E, Smith SR, Mitchell JA, et al. Enhanced weight loss with pramlintide/metreleptin: an integrated neurohormonal approach to obesity pharmacotherapy. Obesity (Silver Spring) 2009;17:1736-43.
Mirza NM, Palmer MG, Sinclair KB, et al. Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American children and adolescents: a randomized controlled trial. Am J Clin Nutr 2013;97:276-285.
Yki-Järvinen H. Nutritional modulation of nonalcoholic fatty liver disease and insulin resistance: human data. Curr Opin Clin Nutr Metab Care 2010;13(6):709-14.
Bradley U, Spence M, Courtney CH, et al. Low-fat versus low-carbohydrate weight reduction diets: effects on weight loss, insulin resistance, and cardiovascular risk: a randomized control trial. Diabetes 2009;58(12):2741-8.
Ross R, Janssen I, Dawson J, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res 2004;12(5):789-798.
O’Hagan C, De Vito G, Boreham CA. Exercise prescription in the treatment of type 2 diabetes mellitus: current practices, existing guidelines and future directions. Sports Med 2013;43:39-49.
Davidson LE, Hudson R, Kilpatrick K, et al. Effects of exercise modality on insulin resistance and functional limitation in older adults: a randomized controlled trial. Arch Intern Med 2009;169(2):122-131.
Williams MA, Haskell WL, et al. American Heart Association Council on Clinical Cardiology; American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation 2007;116:572-584.
Aguilar RB. Evaluating treatment algorithms for the management of patients with type 2 diabetes mellitus: a perspective on the definition of treatment success. Clin Ther 2011;33(4):408-24.
Moore EM, Mander AG, Ames A, et al. Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes Care 2013;36(10):2981-7.