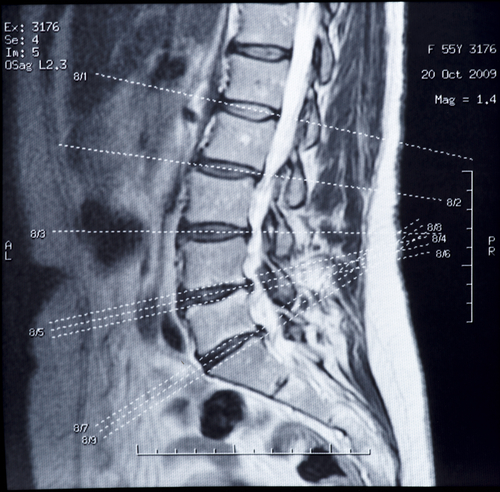
As an Army Doc I saw countless patients with musculoskeletal complaints.
It wasn’t uncommon that someone would come up to be asking for an MRI in order to “find out what is going on“. I often asked them if they were considering Surgey to correct the problem and the most frequent response is “no way, I just want to know what is going on!”
My residency training taught me that an MRI was a great tool to help evaluate the need for surgery and identify a surgically correctable cause for the problem. MRIs can cost over $2000 so they aren’t cheap. Somebody has to pay for it and there should be a good reason to ask for one!
A lot of tests (labs, xrays, CT, and MRI) are like picking your nose in public… what are you going to do with the results?
If an MRI is going to change my management then it is something to consider and may be worth the cost.
However, MRIs are not perfect tests!
I read an article the other day on incidental findings of meniscal damage during knee MRIs. This study evaluated the incidence of meniscal damage in patients who had no knee complaints. They evaluated 991 patients in Framingham, MA without regard to whether or not they had knee complaints and then evaluated whether or not they had any symptoms. They noted that 61% of patients with meniscal tears on MRI didn’t have any knee pain, aching, or stiffness within the previous month.
I like this study because it relays what I’ve been thinking for years…
Just because they find a problem on an MRI it doesn’t mean that it is the cause for the symptoms!
I’ve had numerous patients tell me that they have a herniated disk and they think that is the cause of their back pain. However, on physical examination, I can reproduce their pain by palpation (by pushing on their back). I can also, almost always, dramatically reduce their pain (and in some cases make them pain free) with a prolotherapy injection that doesn’t go anywhere near their intervertebral disk!
Multiple studies have shown that there is no relationship between presence of disk herniation and symptoms.
One study (Boos et al.) evaluated patients with jobs that had high-risk of causing disk herniation (frequent bending, twisting, lifting, vibration, etc). All 96 of these patients were asymptomatic. However, the following ‘abnormalities’ were found:
- 76% had disk herniation
- 17% had minor nerve root compression
- 4% had major nerve root compression
- 85% had Degenerative Disk Disease (DDD)
- 13% had disk extrusion (the jelly in the disk is leaking out)
And none of these patients had ANY symptoms!
If you are middle-aged (average age of 45) and you have an MRI on your lower back, here are the chances you’d have something “abnormal” on your MRI – regardless of symptoms:
- Disk bulge – 38%
- Disk protrusion – 29%
- Disk extrusion – 10%
- Nerve root compression due to herniation – 4%
- Findings of disk bulge, protrusion, or extrusion – 60%
So, MRIs are a valuable and useful tool. BUT we need to exercise discretion when ordering them. It is a rare instance that I need to get an MRI before prolotherapy treatments. I just haven’t found them that helpful.
References:
- Englund M, et al. “Incidental Meniscal Findings on Knee MRI in Middle-Aged and Elderly Persons.” N Engl J Med 2008;359:1108-15
- Jensen MC, et al. “MRI imaging of the lumbar spine in people without back pain.” N Engl J Med – 1994; 331:369-373
- Boden SD et al. “Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects: A prospective investigation.” J Bone Joint Surg Am 1990; 72A:403-408
- Weishaupt D et al. “MRI of the lumbar spine: Prevalence of intervertebral disc extrusion and sequestration, nerve root compression and plate abnormalities, and osteoarthritis of the fact joints in Asymptomatic Volunteers.” Radiology – 1998; 209:661-666
- Boos N, et al. “1995 Volvo Award in clinical science: The diagnostic accuracy of MRI, work perception, and psychosocial factors in identifying symptomatic disc herniations.” Spine – 1995; 20:2613-2625
- Powell MC, et al. “Prevalence of lumbar disc degeneration observed by magnetic resonance in symptomless women.” Lancet – 1986; 2:1366-7
- Boos N, et al. “Natural history of individuals with asymptomatic disc abnormalities in MRI: Predictors of low back pain-related medical consultation and work incapacity.” Spine 2000; 25:1484
- Borenstein G, Boden SD, Wiesel SW, et al. “The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic individuals: A 7-year follow-up study. J Bone Joint [am] 2001; 83:320-34
- Wiesel SW, et al. “A study of computer-associated tomography: I. The incidence of positive CAT scans in asymptomatic group of patients.” Spine 1984;9:549-51
- Wood KB, et al. ‘Magnetic resonance imaging of the thoracic spine. Evaluation of asymptomatic individual s.’ J Bone Joint Surg Am. 1995 Nov;77(11):1631-8
- Jarvik JJ, et al. “The longitudinal assessment of imaging and disability of the back (LAIDBack) Study.” Spine 2001;26: 1158-66.
- Boden SD, et al. “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatci Subjects.” J Bone Joint Surg [AM] 1990; 72:403-408
- Fraser RD, Sandhu A, Gogan WJ. ‘Magnetic resonance imaging findings 10 years after treatment for lumbar disc herniation.’ Spine 1995 Mar 15;20(6):710-4. “The findings of this study indicate that long-term improvement of a patient’s symptoms after treatment of disc herniation may occur with or without resolution of the hernia. This and the similar morphologic findings in the different groups is consistent with the 10-year clinical results after the treatment of disc herniation reported by Weber.”
- Masui T, et al. ‘Natural History of Patients with Lumbar Disc Herniation Observed by Magnetic Resonance Imaging for Minimum 7 Years.’ J Spinal Disord Tech. 2005 Apr;18(2):121-126. “Clinical outcome did not depend on the size of herniation or the grade of degeneration of the intervertebral disc in the minimum 7-year follow-up.”
- Giuliano V, et al. ‘The use of flexion and extension MR in the evaluation of cervical spine trauma: initial experience in 100 trauma patients compared with 100 normal subjects.’ Emerg Radiol. 2002 Nov;9(5):249-53.