Rasmussen Score for Cardiovascular Disease
The Rasmussen Center Score provides a validated risk prediction of having a cardiovascular disease event. Traditional screening for cardiovascular disease is woefully inadequate and identified no better than 50% of patients at risk of having a heart attack.1
The traditional approach to cardiovascular disease risk reduction has been 2-pronged. First, for patients who have already had a cardiovascular event, aggressive intervention is imposed. This is called “secondary prevention” as we are trying to prevent a 2nd heart attack or other cardiovascular event. Secondly, we screen who are considered to be “healthy” for cardiovascular disease “risk factors” and manage these with medications and lifestyle changes if they are considered abnormal.
We need a better way to differentiate those at low risk vs. high risk. The Rasmussen Score for Cardiovascular Disease is a much better test and more accurately identifies patients at risk for cardiovascular disease.
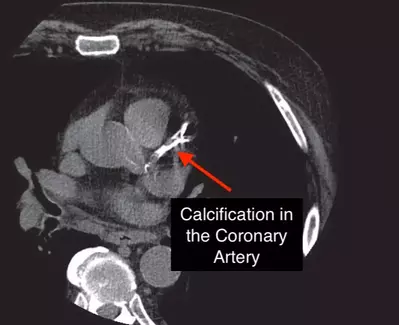
The Rasmussen Score for Cardiovascular Disease is a panel of 10 tests which are easily performed. These tests assess coronary vascular disease and are better able to predict future cardiovascular events such as heart attacks and strokes.
Rasmussen Score for Cardiovascular Disease Methods
Questionnaires were mailed out to 1400 patients who had been previously screened at the Rasmussen Center for Cardiovascular Disease Prevention. The primary focus of the questionnaire was morbid events (heart attack, angina, stroke, CABG, stents, heart failure, and peripheral vascular disease) occurring after their screening tests. 613 questionnaires were returned completed.
There are 10 tests in the Rasmussen Score for Cardiovascular Disease. Arterial elasticity is measured with the CV Profiler and provides the C1 and C2 elasticity index. The scores are age adjusted and are displayed in the table below.
| C1 (large artery) (mL/mmHg x10) | C2 (small artery) (mL/mmHg x100) | ||||||
| Age | Sex | Normal | Borderline | Abnormal | Normal | Borderline | Abnormal |
| <45 | Male | >15 | 12-14.5 | <12 | >7 | 6-6.9 | <6 |
| Female | >12 | 10-11.9 | <10 | >5 | 4-4.9 | <4 | |
| 46-64 | Male | >12 | 10-11.9 | <10 | >6 | 5-5.9 | <5 |
| Female | >10 | 9-9.9 | <9 | >4 | 3.5-3.9 | <3.5 | |
| >65 | Male | >10 | 9-9.9 | <9 | >5 | 4.4-9 | <4 |
| Female | >9 | 8-8.9 | <8 | >3 | 2.5-2.9 | <2.5 | |
| Normal | Borderline | Abnormal | |
| Arterial Elasticity (C1 & C2) | (see table above) | ||
| Resting Blood Pressure | SBP <130 and DBP <85 | SBP 130-139 or DBP 85-89 | SBP >140 or DBP >90 |
| Exercise Blood Pressure | SBP rise <30 and SBP <169 | SBP rise 30-39 or SBP 170-179 | SBP ris >40 or SBP >180 |
| Optic Fundus | A:V Ration >3:5 | A:V ratio <3.5 or Mild A:V crossing changes | A:V ratio <1:2 or A:V nicking |
| Microalbuminuria (mg/mmoL) | <0.6 | 0.61-0.99 | >1.00 |
| Carotid Intima-Media Thickness | >0.90 | 0.90 | <0.90 |
| EKG | No abnormalities | Nonspecific abnormalities | Diagnostic abnormality |
| LV Ultrasound (Echo) | LVIDD/BSA (cm/m2) 2.70 (M); 2.60 (F) and LVM/BSA (gm/m2) <120 (M); <110 (F) | LVIDD/BSA (cm/m2) 2.70-2.89 (M); 2.60-2.79 (F) and LVM/BSA (gm/m2) 120-129 (M); 110-119 (F) | LVIDD/BSA (cm/m2) >2.90 (M); >2.80 (F) and LVM/BSA (gm/m2) >130 (M); >120 (F) |
| BNP | <50 | 51-99 | >100 |
Rasmussen Score for Cardiovascular Disease Scoring System
Each test listed above is scored as Normal, Borderline, or Abnormal. Normal has a score of 0, Borderline = 1, and Abnormal =2. Therefore, if you assign a number to each test then the score ranges from 0 (no evidence of disease) to 20 (strong evidence of disease).
Scores of 0-2 were considered to be absent of cardiovascular disease. A score ranging from 3-5 were considered as evidence of early disease and a score of >6 were considered to have advancing cardiovascular disease.
Results
35 participants experienced a cardiovascular event as defined above between their screening and when they filled out their questionnaires. 26 of these events occurred within the “Advanced Disease” group with a score of >6. 8 events occurred in the “Early Disease” group with a score of between 3 & 5. 1 event occurred in the “no disease” group with a score of 0-2.
Of note, >10% of the morbid events occurred in patients considered to be low-risk by the Framingham Risk Score (FRS). These patients were not identified by the FRS and would, therefore, not been candidates for preventive therapy. The authors stated “Because so few individuals exhibited risk factors in the high-risk category, it is clear that traditional FRS classification is not an adequate discriminator in this population.”
The Hazard Ratio (HR) for the Rasmussen Score for Cardiovascular Disease was greater than the HR for the Framingham Risk Score (FRS).
28% of the participants had a Rasmussen Score for Cardiovascular Disease of 0-2 and there were no cardiovascular events in 6 years of follow up. There was 1 participant in this group that had an event at 8 years but it was noted that his score had increased to 7. These participants were encouraged to follow a healthy lifestyle and return in 5-10 years.
35% of the participants had a score of 3-5 (early disease group) and they had an increased likelihood of having an event but the risk was only 5% after about 4 years. However, 37% of the participants had a score of >6 (advanced disease) and 15% of those participants had an event by 6 years.
Participants in the Early Disease group received more aggressive recommendations and medications were recommended based on current guidelines and asked to return in 3 years for repeat screening. The Advanced Disease group were nearly always treated with medications and asked to return in 1 year.
As is common in the literature, cholesterol and blood pressure measurements do not necessarily discriminate patients who will or will not have an event. The traditional approach of risk-factor based evaluation should be replaced with the early disease assessment as it appears to be much more discriminating.
Discussion
Abnormalities in the cardiovascular system exhibit far before a cardiovascular event. Therefore, if we can screen for and identify these abnormalities and work to reduce them then we should be able to reduce cardiovascular disease events. The Rasmussen Score for Cardiovascular Disease is much more sensitive for cardiovascular disease risk and will allow us to identify more patients at an earlier stage where our efforts are both better and more cost effective.
This testing takes approximately 1 hour to perform and costs approximately $600. Some of the testing may be covered by insurance. The return on investment of this modest-cost testing should be quite high.
References
- J Am College of Cardiology 2017;70(24):2979-91
- J Am Society of Hypertension 2011;5:401