As discussed previously, apoB-containing LDL particles exist as a heterogeneous collection of variable sized particles, from small to large. There are technologies that size or measure peak particle diameters (in Angstroms or nanometers).1,2
- Phenotype or Pattern A – Predominant LDL species is large. This is the one you want!
- Phenotype or Pattern B (not to be confused with apoB) – Predominant LDL species is small3,4
Small, dense LDL (sdLDL), or more accurately small, dense LDL-cholesterol (sdLDL-C), is the cholesterol mass trafficked within the small LDL particles. It takes 40-70% more smaller LDLs than larger ones to traffic a given cholesterol mass, hence increased sdLDL-C is usually associated with high numbers of small LDL particles and total LDL-P.5
By definition, smaller lipoproteins are denser than larger species as there is more protein relative to the lipid content. Hence, the redundant term small LDL need not be always written as small, dense LDL. As sdLDL often traffics lipoprotein associated phospholipase A2 (Lp-PLA2), it is more prone to oxidative forces than large buoyant LDL and thus is likely more atherogenic.6,7
Studies have shown that elevated sdLDL particle concentration is associated with increased risk for coronary heart disease (CHD) even in the presence of optimal LDL-C values.3,5,8-10 However, when sdLDL-P concentrations are high, so is total LDL-P (apoB). sdLDL mass (particle number) plays a more important role in the progression of CHD than the LDL size, and sdLDL concentration serves as a powerful surrogate marker for CHD risk.8 By using the ratio of sdLDL-C to total LDL-C, it is easy to estimate the percentage of the total LDL-C that is made up of small dense particles.
Clinical Impact
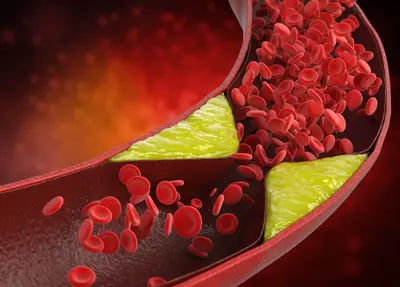
Small, dense LDL particles are more easily modified by reactive oxygen species than larger LDL particles. They are more susceptible to oxidation, have a reduced affinity for the LDL receptors, and have increased clearance by scavenger receptors resulting in increased foam cell formation.5-8,11
Small LDLs also have a longer half-life than larger LDL particles. That means they stick around longer. Plus, their very small size may permit easier penetration of the endothelial wall.11
Moreover, small LDL particles are thought to be more readily retained in the artery wall, having a higher affinity for the proteoglycans that reside in this area.12,13
sdLDL and Blood Sugar
Small LDL particles may be observed in association with insulin resistance (IR) disorders such as obesity, the metabolic syndrome and prediabetes, and type 2 diabetes mellitus (T2DM), or in patients with renal dysfunction.14-32 Plasma/serum sdLDL levels are highest in the morning before breakfast; postprandial sdLDL levels are lower than fasting sdLDL, in part due to CETP-mediated TG-enrichment.33 After glucose ingestion, sdLDL levels are decreased.34 Trans-fat intake has also been shown to increase sdLDL levels.35
In addition to cross-sectional studies that have demonstrated an association between a predominance of small LDLs and increased risk for cardiovascular disease and diabetes mellitus, a reduction in LDL size has also been reported in patients with acute myocardial infarction, with angina pectoris as well as in those with non-coronary forms of atherosclerosis.36-40
sdLDL & Cardiovascular disease
If unadjusted for particle number, LDL size appears to be an important predictor of cardiovascular events and progression of coronary artery disease. Indeed, the predominance of small LDL was (in 2001) accepted as an emerging cardiovascular risk factor by the National Cholesterol Education Program Adult Treatment Panel III.41
However, data emerging from more recent studies shows that once adjusted for total LDL-P, LDL size is no longer an independent predictor of risk.39,42,43
Nevertheless, high sdLDL values, with elevated triglyceride levels and low high density lipoprotein (HDL)-C concentrations (also defined as disorders of the TG/HDL-C axis), constitute the “atherogenic lipoprotein phenotype (ALP),”3,9,41 a form of atherogenic dyslipidemia that is a feature of Type-2 Diabetes and the metabolic syndrome.11,13,41
The most important role of sdLDL in drug-naïve patients is as a marker of insulin resistance. Because smaller LDLs are cholesterol depleted, LDL-C or total cholesterol may not be increased in patients with diabetes, except for a slight increase of LDL-C in women.17
Subjects with a predominance of sdLDL have a greater than two-fold increased risk for developing type-2 diabetes mellitus, independent of age, sex, glucose tolerance and body mass index. Increases of peak LDL size were associated with a 16% decrease in the risk of developing Type-2 Diabetes.19
It has also been shown that patients with the insulin resistance syndrome have an elevated prevalence of the LDL “pattern B” phenotype20 and this has been confirmed for diabetes, in both men and women.21,22,44 In addition, when individuals were categorized as insulin-sensitive, insulin-resistant, or type 2 diabetic, more severe states of insulin resistance were associated with smaller LDL particle size.23,45 The reduction in LDL size occurs long before any glucose perturbation.
Therefore, the presence of both small LDL size and small LDL-P can be predictors of future T2DM.46
When Hulthe et al.47 assessed the prevalence of metabolic syndrome (using the World Health Organization definition) in a population-based sample of 58-year-old healthy men, the researchers found that LDL size was significantly smaller in subjects with the metabolic syndrome, compared to those without it.
In addition, subjects with pattern B had significantly higher mean values for body mass index, blood pressure, heart rate, serum cholesterol, triglyceride levels, and plasma insulin, and lower HDL levels compared with subjects with pattern A.
Subjects with pattern B also had a higher prevalence of moderate to large plaques in the carotid artery compared with subjects with pattern A. Decreasing LDL peak particle size was significantly associated with increasing carotid intima media thickening (CIMT) of the common carotid artery, the carotid artery bulb, and the common femoral artery. There was a statistically significant association between plaque occurrence and size and the LDL peak particle diameter in both the carotid and femoral arteries.45
Increased carotid intima media thickness (CIMT) is considered a reliable surrogate marker of early atherosclerosis and has been shown to correlate significantly with the presence of CHD and to predict coronary events.24,48,49 Berneis et al. (2005) found that LDL size was significantly associated with carotid IMT in patients with T2DM. LDL size was the second strongest predictor of IMT, after smoking, when compared with nine other cardiovascular risk factors, and was the strongest of all lipid parameters that were evaluated.50
However, this study was not adjusted for apoB or LDL-P. In another study, increased sdLDL-C level was a significant predictor of acute ischemic stroke (AIS) and in-hospital short-term mortality after AIS, a finding that persisted after adjustment for conventional risk factors (but not apoB). These results indicate that sdLDL predicts both AIS onset and consecutive short-term mortality, independent of traditional risk factors.51
Studies have demonstrated independent associations of both hepatic steatosis (HS) and the metabolic syndrome with LDL particle size, even after adjustment for apoB.12 LDL particle size is closely related with serum levels of TG, HDL cholesterol, and insulin resistance.45
Cholesterol Particles
Large amounts of plasma TG are carried or transported by very low-density lipoprotein (VLDL) from liver or chylomicrons from the gut. These particles typically undergo delayed catabolism in insulin resistant patients, which allows cholesteryl ester transfer protein (CETP) to exchange the TG for cholesteryl ester (CE) in intermediate-density lipoproteins (IDLs), LDLs and HDLs.52
These latter particles thus become TG-rich and CE-poor. TG-rich HDL and LDL then undergo additional hydrolysis by hepatic lipase (a form of lipoprotein lipase or LPL), creating smaller HDL and LDL species. The very small HDL is further degraded and its structural apoA-I is excreted by the kidney, leading to decreased serum apoA-I, HDL-P and HDL-C.30 As for cardiovascular risk, both quality (i.e., LDL peak particle size) and quantity (apoB or LDL-P) of LDL were reported to be important equally and additively.53 It should also be noted that CETP activity results in CE enrichment of VLDL and postprandial chylomicron remnants.
The smaller LDL particle size in the subjects with hepatic steatosis alone could be explained by the concept of hepatic insulin resistance, which occurred primarily31 and more evidently54 than peripheral insulin resistance. Hepatic fat accumulation in HepG2 cells was found to induce serine phosphorylation of insulin receptor substrate (IRS)-1 and endoplasmic reticulum (ER) stress, as previously reported by the authors.32 The ER stress, in turn, led to the suppression of insulin receptor signaling, causing hepatic insulin resistance with no evident peripheral insulin resistance.
How To Reduce sdLDL
Although not specified as a goal of therapy in any guidelines, sdLDL levels may be reduced through a variety of different treatment options:
- Diet (reducing intake of simple sugars and refined carbohydrates),11,35,43 exercise, and lifestyle modification (weight loss, smoking cessation).
- Statin therapy, the standard first line drug for elevated apoB or sdLDL-C, can effectively reduce the number of LDL particles (the primary goal) but does not generally influence their size distribution. Although statins may increase sdLDL levels when triglycerides are low, this is likely of no concern if apoB and LDL-P reductions are substantial.
- Other medications such as niacin, fenofibrate, high-dose omega-3 fatty acids, or a combination of medications (niacin + statin, fenofibrate + statin, or omega-3 + statin) can decrease sdLDL levels; however, only statin plus niacin reduces LDL-P beyond statin monotherapy.55,56
- Treating glycemic abnormalities in diabetes and insulin resistance patients with insulin therapy can decrease sdLDL particles by reducing triglycerides in TG-rich lipoproteins. Thiazolidinedione insulin sensitizers, such as pioglitazone (off-label use) may have a similar action.
References
- Menys VC, Liu Y, Mackness M, et al. Measurement of plasma small-dense LDL concentration by a simplified ultracentrifugation procedure and immunoassay of apolipoprotein B. Clinica Chimica Acta 2003;334:95–106
- Hirano T, Ito Y, Yoshino G. Measurement of small dense low density lipoprotein particles. J Atheroscler Thromb 2005;12:67-72.
- Austin MA, King MC, Vranizan KM, et al. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation 1990;82:495–506.
- Krauss RM, Burke DJ. Identification of multiple subclasses of plasma low density lipoproteins in normal humans. J Lipid Res 1982;23:97-104.
- Taskinen MR. LDL-cholesterol, HDL-cholesterol or triglycerides – which is the culprit? Diab Res Clin Prac 2003;61:S19-S26.
- De Graaf J, Hak-Lemmers HDL, Hectors MP, et al. Enhanced susceptibility to in vitro oxidation of the dense low-density lipoprotein subfraction in healthy subjects. Arterioscler Thromb 1991;11:298-306.
- Tribble DL, Holl LG, Wood PD, et al. Variations in oxidative susceptibility among six low-density lipoprotein subfractions of differing density and particle size. Atherosclerosis 1992;93:189-199.
- Koba S, Hirano T, Kondo T et al. Significance of small dense low-density lipoproteins and other risk factors in patients with various types of coronary heart disease. Am Heart J 2002;144(6):1026-35.
- Rizzo M, Berneis K. Lipid triad or atherogenic lipoprotein phenotype: a role in cardiovascular prevention? J Atheroscler Thromb 2005;12:237–239.
- Sattar N, Petrie JR, Jaap AJ. The atherogenic lipoprotein phenotype and vascular endothelial dysfunction. Atherosclerosis 1998;138:229–235.
- Musunuru K. Atherogenic dyslipidemia: Cardiovascular risk and dietary intervention. Lipids 2010;45:907-914.
- Anber V, Griffin BA, McConnell M, et al. Influence of plasma lipid and LDL-subfraction profile on the interaction between low density lipoprotein with human arterial wall proteoglycans. Atherosclerosis 1996; 124: 261-271.
- Olin-Lewis K, Krauss RM, La Belle M, et al. ApoC-III content of apoB-containing lipoproteins is associated with binding to the vascular proteoglycan biglycan. J Lipid Res 2002;43:1969-1977.
- Kim DS, Kim YK, et al. Low-density lipoprotein particle size in hepatic steatosis and metabolic syndrome. Diabetol Metab Syndr 2010;2:18.
- Grundy SM, Cleeman JI, Daniels SR, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association / National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–2752.
- Syvanne M, Taskinen MR. Lipids and lipoproteins as coronary risk factors in non-insulin-dependent diabetes mellitus. Lancet 1997;350(Suppl 1):SI20–SI23.
- U.K. Prospective Diabetes Study 27. Plasma Lipids and lipoproteins at diagnosis of NIDDM by age and sex. Diabetes Care 1997;20:1683–1687.
- Friedlander Y, Kidron M, Caslake M, et al. Low density lipoprotein particle size and risk factors of insulin resistance syndrome. Atherosclerosis 2000;148:141–149.
- Austin MA, Mykkanen L, Kuusisto J, et al. Prospective study of small LDLs as a risk factor for non-insulin dependent diabetes mellitus in elderly men and women. Circulation 1995;92:1770–1778.
- Reaven GM, Chen YD, Jeppesen J, et al. Insulin resistance and hyperinsulinemia in individuals with small dense low-density lipoprotein particles. J Clin Invest 1993;92:141–146.
- Feingold KR, Grunfeld C, Pang M, et al. LDL subclass phenotypes and triglyceride metabolism in non-insulin dependent diabetes. Arterioscler Thromb 1992;12:1496–1502.
- Selby JV, Austin MA, Newman B, et al. LDL subclass phenotypes and the insulin resistance syndrome in women. Circulation 1993;88:381–387.
- Garvey WT, Kwon S, Zheng D, et al. Effects of insulin resistance and type 2 diabetes on lipoprotein subclass particle size and concentration determined by nuclear magnetic resonance. Diabetes 2003;52:453–462.
- Goya K, Kitamura T, Inaba M, et al. Risk factors for asymptomatic atherosclerosis in Japanese type 2 diabetic patients without diabetic microvascular complications. Metabolism 2003;52:1302–1306.
- Niskanen L, Rauramaa R, Miettinen H, et al. Carotid artery intima-media thickness in elderly patients with NIDDM and in nondiabetic subjects. Stroke 1996;27:1986–1992.
- Rizzo M, Barbagallo CM, Noto D, et al. Diabetes, family history and extension of coronary atherosclerosis are strong predictors of adverse events after PTCA: a one year follow-up study. Nutr Metab Cardiovasc Dis 2005;15:361–367.
- Haffner SM, Mykkanen L, Robbins D, et al. A preponderance of small dense LDL is associated with specific insulin, proinsulin and the components of the insulin resistance syndrome in nondiabetic subjects. Diabetologia 1995;38:1328–1336.
- Garin MC, Kalix B, Morabia A, et al. Small, dense lipoprotein particles and reduced paraoxonase-1 in patients with the metabolic syndrome. J Clin Endocrinol Metab 2005;90:2264–2269.
- Slapikas R, Luksiene D, Slapikiene B, et al. Prevalence of cardiovascular risk factors in coronary heart disease patients with different low-density lipoprotein phenotypes. Medicina (Kaunas) 2005;41:925–931.
- Ito MK. The metabolic syndrome: pathophysiology, clinical relevance, and use of niacin. Ann Pharmacother 2004;38(2):277-285.
- Kim SP, Ellmerer M, Van Citters GW, et al. Primacy of hepatic insulin resistance in the development of the metabolic syndrome induced by an isocaloric moderate-fat diet in the dog. Diabetes 2003;52(10):2453-2460.
- Kim DS, Jeong SK, Kim HR, et al. Effects of triglyceride on ER stress and insulin resistance. Biochem Biophys Res Commun 2007;363(1):140-145.
- Ogita K, Ai M, Tanaka A, Ito Y, et al. Circadian rhythm of serum concentration of small dense low-density lipoprotein cholesterol. Clin Chim Acta 2007;376(1-2):76-41.
- Ogita K, Ai M, Tanaka A, et al. Serum concentration of small dense low-density lipoprotein-cholesterol during oral glucose tolerance test and oral fat tolerance test. Clin Chim Acta 2008;387(1-2):76-41.
- Jones JL, Comperatore M, Barona J, et al. A mediterranean-style, low-glycemic load diet decreases atherogenic lipoproteins and reduces lipoprotein(a) and oxidized low-density lipoprotein in women with metabolic syndrome. Metabolism 2011; Sep 22 [e-pub ahead of print].
- Ai M, Otokowaza S, Asztalos BF, et al. Small dense LDL cholesterol and coronary heart disease: results from the Framingham Offspring Study. Clin Chem 2010;56(6):967-976.
- Maeda S, Nakanishi S, Yoneda M, et al. Associations between small dense LDL, HDL subfractions (HDL2, HDL3) and risk of atherosclerosis in Japanese Americans. J Atheroscler Thromb 2011; Dec 21: e-pub ahead of print.
- Suh S, Park HD, Kim SW, et al. Smaller mean particle size and higher proportion of small dense LDL in Korean type 2 diabetic patients. Diabetes Metab J 2011;35(5):536-542.
- Mora S, Szklo M, Otvos JD, et al. LDL particle subclasses, LDL particle size and carotid atherosclerosis in the Multi-ethnic Study of Atherosclerosis (MESA). Atherosclerosis 2007;192:211-217.
- Toft-Peterson AP, Tilsted HH, Aaroe J, et al. Small dense LDL particles – a predictor of coronary artery disease evaluated by invasive and CT-based techniques: a case-control study. Lipids Health Dis 2011;10:21.
- National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Third report of the National Cholesterol Education Program(NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–3421.
- Otvos JD, Collins D, Freedman DS, et al. Low density lipoprotein and high density lipoprotein particle subclasses predict coronary events and are favorably changed by gemfibrozil therapy in the Veterans Affairs High-Density Intervention trial. Circulation 2006;113:1556-1563.
- Cromwell WC, Otvos JD, Keyes MJ, et al. LDL particle number and risk of future cardiovascular disease in the Framingham Offspring Study—Implications for LDL management. J Clin Lipidol 2007;1:583–592.
- Krauss RM. Dietary and genetic probes of atherogenic dyslipidemia. Arterioscler Thromb Vasc Biol 2005; 25: 2265–2272.
- Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol 1997;146:483–494.
- Frazier-Wood AC, Garvey TW, Dall T, et al. Opportunities for using lipoprotein subclass profile by nuclear magnetic resonance spectroscopy in assessing insulin resistance and diabetes prediction. Metab Syndr Relat Disord 2012;10(4):244-51.
- Hulthe J, Bokemark L, Wikstrand J, et al. The metabolic syndrome, LDL particle size, and atherosclerosis: the Atherosclerosis and Insulin Resistance (AIR) study. Arterioscler Thromb Vasc Biol 2000;20:2140–2147.
- Craven TE, Ryu JE, Espeland MA, et al. Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study. Circulation 1990;82:1230–1242.
- Wofford JL, Kahl FR, Howard GR, et al. Relation of extent of extracranial carotid artery atherosclerosis as measured by B-mode ultrasound to the extent of coronary atherosclerosis. Arterioscler Thromb 1991;11:1786–1794.
- Berneis K, Jeanneret C, Muser J, et al. Low-density lipoprotein size and subclasses are markers of clinically apparent and non-apparent atherosclerosis in type 2 diabetes. Metabolism 2005;54:227–234.
- Zeljkovic A,Vekic J, Spasojevic-Kalimanovska V, et al. LDL and HDL subclasses in acute ischemic stroke: Prediction of risk and shortterm mortality. Atherosclerosis 2010;210(2):548-54.
- Tall AR. Plasma cholesteryl ester transfer protein. J Lipid Res 1993;34(8):1255-1274.
- Rizzo M, Berneis K. Low-density lipoprotein size and cardiovascular risk assessment. QJM 2006;99(1):1-14.
- Samuel VT, Liu ZX, Qu X, et al. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem 2004;279(31):32345-32353.
- Backes JM, Gibson CA, Effect of lipid-lowering drug therapy on small-dense low-density lipoprotein. Ann Pharmacother 2005;39:523-526.
- Maki KC, Bays HE, Dicklin MR et al. Effects of prescription omega-3 acid ethyl esters, coadministered with atorvastatin, on circulating levels of lipoprotein particles, apolipoprotein CIII, and lipoprotein-associated phospholipase A2 mass in men and women with mixed dyslipidemia. J Clin Lipidol 2011;5(6):483-92