In contrast to the other water soluble vitamins, cobalamin is stored in the body (~4-5 mg).
There are 2 primary forms with which most people supplement: cyanocobalamin and methylcobalamin. Hydroxycobalamin is a stable form that is converted to the active, methylcobalamin form.
How it absorbs
When taken orally, Vitamin B12 binds to intrinsic factor which is produced in the stomach. The complex of Vitamin B12 & intrinsic factor is absorbable. Without intrinsic factor we cannot absorb Vitamin B12 through the gastrointestinal tract.
This issue is the most common reason that people don’t have adequate levels. We also commonly see deficiency in vegetarians and vegans because there are not good plant sources of B12.
Autoimmune attack of the gastric parietal cells destroys the bodies ability to produce intrinsic factor.
The B12-Intrinsic Factor complex is absorbed in the ileum of the small intestine. Some people may also have a gut disorder that could decrease the absorption of B12.
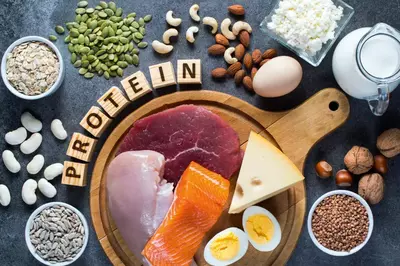
Good sources
This vitamin is not found in plants! It is synthesized only by microorganisms. Animals obtain cobalamin from intestinal flora or by eating the meats of other animals. Especially liver, whole milk, eggs, oysters, fresh shrimp, pork, and chicken.
DRI: 1.8-2.4 mg/d
Our sublingual methylcobalamin is 2.5mg per day and also contains 5-MTHF 1mg. We also give methylcobalamin as an injection and it is included in several of our IV nutritional formulas.
Functions:
Vitamin B12 (cobalamin) is essential for 2 enzymatic reactions: synthesis of methionine and isomerization of methylmalonyl CoA that arises from odd fatty acid chains. Cobalamin converts some forms of TetraHydroFolate (THF) to the active form (5-MTHF). If cobalamin is deficient, the inactive forms build up and cannot be converted. Therefore, cobalamin deficiency can resemble folic acid deficiency and vice versa. This process is further discussed on the Methylation post.
Check out our podcast about methylation as well.
- Cofactor in mitochondrial respiratory chain to produce energy via ATP
- Cofactor in methionine synthase, an enzyme that methylates homocysteine to form methionine (see methylation post)
- Cofactor in the synthesis of S-Adenosylmethionine (SAMe) which synthesizes neurotransmitters
- Cofactor in the L-methylmalonyl-CoA mutase which synthesizes succinyl-CoA which metabolizes proteins and fats
- Cofactor in folate metabolism (prevents folate derivatives from staying in non-bioactive form)
- Cofactor in the metabolism of odd-chain fatty acids
- Cofactor in the metabolism of branched chain amino acids (leucine, isoleucine, and valine)
- Cofactor in the formation of red blood cells (RBCs) (succinyl-CoA is required for hemoglobin)
- Cofactor in the formation of white blood cells (WBCs)
- Modulates melatonin secretion via its role as a methyl donor, thus normalizing circadian rhythms
- Key role in methylation and synthesis of DNA (low B12 causes hypomethylation of DNA)
- Cofactor in donating methyl groups to myelin sheath around nerves (via SAMe)
- Reduces neuropathic pain
- Raises cysteine and glutathione (GSH) levels
- Scavenges nitric oxide (NO); inhibits nitric oxide synthase
- Repletion improves treatment response in depression
- Inhibits proliferations of malignant cells in vivo
- May enhance efficacy of methotrexate
- Protects retinal neurons against N-methyl-D-aspartate receptor mediated glutamate neurotoxicity
Deficiencies:
Pernicious anemia. Deficiency is most often due to an inability to absorb the vitamin rather than an inadequate amount in the diet. Vitamin B12 deficiency can also lead to CNS symptoms. Folic acid supplementation can correct the anemia associated with vitamin B12 deficiency but not the CNS effects. Make sure you know which is deficient!
Deficiency causes excess methylmalonic acid which decreases fatty acid synthesis for nerve cells.
Toxicity: None known
I often look at methylcobalamin as a ‘litmus test’ of the quality of nutritional supplements. It is slightly more expensive to produce so it helps me to understand how important quality may be to the manufacturer. I only recommend methylcobalamin, adenosylcobalamin, or hydroxycobalamin supplementation whether it be orally or injectable. Most traditional doctors use the cyanocobalamin version in their ‘B12 injections.’
Cyanocobalamin has a cyanide molecule attached to it. Do you want to inject your body with cyanide?
We recommend a supplement with B12 (methycobalamin) in a sublinqual form. Sublinqual forms are absorbed directly into the blood system so we don’t have to worry about intrinsic factor and gut health for absorption.
Vitamin B12 refers primarily to cyanocobalamin (they are used interchangeably), but also to several other cobalamins which possess similar nutritional properties. Vitamin B12 is synthesized by bacteria and is found in soil and in contaminated water. The average Western diet contains 5 to 15 μg/day of vitamin B12, and exceeds the recommended dietary allowance of 2 μg/day.1,2 The primary dietary sources of vitamin B12 are in foods of animal derivation (meat, eggs, and milk). Absorption of vitamin B12 occurs when it is bound to intrinsic factor from the stomach parietal cells.2 Vitamin B12 deficiency is rare in individuals who consume animal products unless there is an underlying vitamin B12 malabsorption condition. Strict vegetarians and babies of mothers who are strict vegetarians are at an increased risk for developing anemia.1-3 The body stores a large amount of vitamin B12 (i.e., 2-5 mg), primarily in the liver. It takes 2 to 5 years to develop a vitamin B12 deficiency even in the presence of severe malabsorption.1,2 However, it is estimated that 5% to 40% of the elderly population have B12 deficiency,4 probably due to reduced intrinsic factor production.2,5
Clinical Interpretation
Vitamin B12 deficiency, related to poor intestinal B12 absorption or dietary deficiency, is associated with pernicious anemia, cardiovascular disease, cancer, and neurodegenerative disorders.6 A cobalamin-dependent reaction involves the synthesis of methionine from homocysteine using methylcobalamin as a cofactor. One hypothesis is that this reaction has primary importance in vitamin B12 and folate deficiencies. A deficiency of either vitamin impairs tetrahydrofolate production.7 In megaloblastic anemia patients, this causes a defect in DNA synthesis that prevents cell division in the marrow. RNA synthesis and cytoplasmic component synthesis are not affected, which results in the production of large erythrocytes.1,2 In addition, a deficiency of either vitamin will result in homocysteine accumulation.1
A cobalamin deficiency may also cause increased methylmalonyl-CoA and its hydrolysis product, methylmalonic acid (MMA).1,8 MMA is regarded as a primary marker of cobalamin deficiency and there are increasing data that high homocysteine concentrations may contribute to occlusive vascular disease, cognitive dysfunction, and adverse pregnancy outcomes and malformations.7,9,10 Functional vitamin B12 deficiency in vegetarians may contribute to hyperhomocysteinemia in this population.3
Homocysteine and MMA are sensitive markers of cobalamin status and are used for the diagnosis and follow-up of cobalamin deficiency. Homocysteine is also elevated in folate deficiency and is used as an indicator of this deficiency state. MMA is a sensitive but specific marker of cobalamin function, although renal dysfunction may also cause significantly elevated MMA concentrations.9 Homocysteine is elevated in both folate and cobalamin deficiencies and also in pathologic states such as renal failure, thyroid dysfunction, coronary artery disease, and the acute phase after a cardiovascular event.7,9,10
A vitamin B12 test is used to check for megaloblastic anemia and to identify the cause of certain dementias or other nervous system symptoms (i.e., peripheral neuropathy). Vitamin B12 is usually measured at the same time as folic acid because a megaloblastic anemia may be caused by a deficiency of either vitamin. The two metabolic markers MMA and homocysteine are generally considered more sensitive indicators of vitamin B12 status than are plasma cobalamin levels.9,11 Homocysteine is an intermediary amino acid formed during the metabolism of methionine, an essential amino acid derived from protein. Hyperhomocysteinemia (> 15 µmol/L) induces vascular endothelial dysfunction and is considered to be an independent risk factor for atherosclerosis and cardiovascular disease (CVD). Treatment with folic acid, pyridoxine hydrochloride (vitamin B6), and vitamin B12 has been shown to reduce homocysteine levels in intervention studies and to reverse endothelial dysfunction independent of the effect of lowering homocysteine levels.11- 14 Therefore, it is reasonable to propose that lowering homocysteine levels with folic acid and B vitamin supplements may help to decrease hyperhomocysteinemia.7,10-12
The most common screening test for vitamin B12 deficiency is the measurement of total plasma or serum
vitamin B12. Although cutoffs vary among assays and laboratories, a total vitamin B12 concentration < 148 pmol/L (< 200 pg/mL) is commonly considered indicative of vitamin B12 deficiency.1,2,5 High levels of vitamin B12 can occur in liver disease (such as cirrhosis or hepatitis) and some types of leukemia. However, the vitamin B12 test is not usually used to diagnose these conditions. Rarely, high levels may be found in obese or diabetes patients.
Causes of vitamin B12 deficiency include malabsorption, low dietary intake, strict vegetarian diet, pernicious anemia, gastric bypass or gastrectomy, ileal disease or resection, pancreatic insufficiency, absence or dysfunction of intrinsic factor, bacterial overgrowth, and impaired utilization.1,2
The most common symptoms of anemia include fatigue, shortness of breath, and palpitations. Vitamin B12 deficiency anemia may also be caused by a lack of intrinsic factor—pernicious anemia. The patient’s digestive system cannot absorb B12 properly. Signs and symptoms of pernicious anemia may include: a sore mouth and/or tongue, weight loss, pale or yellowish skin, diarrhea (sporadic), menstrual problems, greater susceptibility to infections.1,11 If the deficiency continues untreated the patient may have neurological signs and symptoms (e.g., tingling or numbness of the fingers or toes, general muscle weakness, difficulty walking, irritability, confusion, forgetfulness, tender calves).11
Who should be tested?
- Pernicious anemia patients; approximately 60% have low RBC folate levels because vitamin B12 is required for normal transfer of MTHF from plasma to RBCs
- Patients with elevated homocysteine
- Patients post gastric bypass
- Patients suspected of having macrocytic (megaloblastic) anemia; symptoms are weakness, fatigue, difficult concentration, irritability, headache, palpitations, and shortness of breath
- Patients with peripheral arterial disease (PAD)
- Patients with cognitive dysfunction, depression, mental changes, dementia, or insomnia
- Patients with inadequate intake (e.g., malnutrition, malabsorption), increased demands (e.g., pregnancy, infancy), diseases associated with rapid cellular proliferation (hemolysis, leukemia, exfoliative dermatitis), jejunal diseases, short-bowel syndrome, and bacterial overgrowth
- Patients on a strict vegetarian diet who may be deficient
- Patients with chronic inflammatory bowel diseases
- Patients with alcoholism, which may cause significant malnutrition and folate transport defects
- Drugs (e.g., sulfasalazine, phenytoin, primidone, phenobarbital, oral contraceptives, methotrexate, triamterene) may reduce folic acid absorption and enhance folate deficiencies when patients on these drugs are not receiving supplementation
Treatment Considerations
Vitamin B12 and folate deficiencies usually require lifelong treatment with supplements. Lack of gastric intrinsic factor necessitates vitamin B12 injections. Once the diagnosis of vitamin B12 deficiency has been confirmed efficient treatment can be ensured either by injections every 2-3 months or by a daily dose of 1 mg vitamin B12.11 Patients who are taking metformin are at increased risk for vitamin B12 deficiency and may benefit from sublingual vitamin B12 supplementation.15 Vitamin B12 administration will increase red blood cell production, which may increase the need for iron supplementation as well.11
References
- Snow CF: Laboratory diagnosis of vitamin B12 and folate deficiency; a guide for the primary care physician. Arch Intern Med 1999;159:1289-1298
- Jordan NS: Hematology: Red and white blood cell tests. In: Traub SL, ed: Basic Skills in Interpreting Laboratory Data, 2nd ed. Bethesda, MD: American Society of Health System Pharmacists, 1996. pp. 302-304.
- Herrmann W, Schorr H, Purschwitz K, et al. Total homocysteine, vitamin B12, and total antioxidant status in vegetarians. Clin Chem 2001;47(6):1094–1101.
- Loikas S, Koskinen P, Irjala K, et al. Vitamin B12 deficiency in the aged: a population-based study. Age and Ageing 2007;36:177–183.
- Miller JW. Assessing the association between vitamin B12 status and cognitive function in older adults. Am J Clin Nutr 2006;84:1259–60.
- Ryan-Harshman M, Aldoori W. Vitamin B12 and health. Can Fam Physician 2008;54(4):536-41.
- Stanger O, Herrmann W, Pietrzik K, et al. Clinical use and rational management of homocysteine, folic acid, and B vitamins in cardiovascular and thrombotic diseases. Z Kardiol 2004;93:439-453
- Christen WG, Glynn RJ, Chew EY, et al. Folic acid, pyridoxine, and cyanocobalamin combination treatment and age-related macular degeneration in women. The Women’s Antioxidant and Folic Acid Cardiovascular Study. Arch Intern Med 2009;169(4):335-341.
- Monsen AL, Ueland PM. Homocysteine and methylmalonic acid in diagnosis and risk assessment from infancy to adolescence. Am J Clin Nutr 2003;78:7-21.
- Selhub J. The many facets of hyperhomocysteinemia: studies from the Framingham cohorts. J Nutr 2006;136:1726S-1730S.
- Hvas AM, Nexo E. Diagnosis and treatment of vitamin B12 deficiency. An update. Haematologica 2006;91:1506-1512.
- Homocysteine Lowering Trialists’ Collaboration. Dose-dependent effects of folic acid on blood concentrations of homocysteine: a metaanalysis of the randomized trials. Am J Clin Nutr 2005;82(4):806-812.
- Moens AL, Vrints CJ, Claeys MJ et al. Mechanisms and potential therapeutic targets for folic acid in cardiovascular disease. Am J Physiol Heart Circ Physiol 2008;294:H1971-H1977.
- Title LM, Cummings PM, Giddens K, et al. Effect of folic acid and antioxidant vitamins on endothelial dysfunction in patients with coronary artery disease. J Am Coll Cardiol 2000;36(3):758-65.
- Moore EM, Mander AG, Ames A, et al. Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes Care 2013;36(10):2981-7.